Home » Medical Procedure » Advanced Neuromodulation & Functional Neurosurgical Procedures
Advanced Neuromodulation & Functional
Neurosurgical Procedures
at Wockhardt Hospitals
Wockhardt Hospitals now offer advanced, life-changing treatments for patients with neurological conditions that are resistant to conventional therapies. These breakthrough interventions, grounded in the evolving field of Functional Neurosurgery, are designed to restore lost neurological functions through minimally invasive procedures that precisely modulate brain and spinal cord circuits. By targeting the underlying neural pathways, these therapies can significantly improve functional outcomes, enhance quality of life, and reduce dependence on long-term medications.
Request an Appointment
Our Approach
- Expert Functional Neurosurgeon with experience in high precision and technology-oriented Brain and Spine circuit surgeries
- Thorough patient selection with detailed preoperative workup
- Multidisciplinary collaboration (Neurosurgery, Neurology, Psychiatry, Rehab, Pain, Speech specialists, Urology)
- Personalized neurosurgical and post-implant programming
- Long-term follow-up and optimization.
- Dedicated Parkinson’s clinic every Friday 2-4 pm with all the expertise in one clinic so that all the problems of the patient are addressed in one appointment and a holistic care is given.
Dr. Manish Baldia
MCh (CMC Vellore), EEPIN (London)
Functional Neurosurgeon | Parkinson’s and Movement Disorder Specialist | Neuromodulation Specialist
Wockhardt Hospital, Mumbai Central
Contact: 082911 01001
Dr. Manish Baldia is a highly skilled Functional Neurosurgeon with extensive experience in both advanced neuromodulation surgeries and post-operative device programming. He has gained his neurosurgical experience over 12 years from the prestigious Christian Medical College Vellore where the first Neuroscience department was started in South-Asia. He did his fellowship in Functional Neurosurgery and Neuromodulation course from London. With a specialized focus on treating complex neurological disorders such as Parkinson’s disease, dystonia, epilepsy, spasticity, urological problems and chronic pain, he combines surgical expertise with deep knowledge of neurophysiology and neuromodulation technology. Dr. Baldia is proficient in troubleshooting and optimizing implanted devices like Deep Brain Stimulators (DBS), Spinal Cord Stimulators (SCS), Baclofen pumps, and other neurostimulators, offering comprehensive, patient-specific care. His multidisciplinary approach ensures not only surgical precision but also long-term functional outcomes and quality of life improvements.
Overview of Advanced Treatments
What is Neuromodulation?
Neuromodulation is a revolutionary minimally invasive surgical technique that uses targeted electrical stimulation to alter nerve activity. It is transforming care for patients with movement disorders (Tremors, Parkinson’s Huntingtons’s), epilepsy, stroke, chronic pain, spinal cord injury, ventilator patients, urine problems and even certain psychiatric conditions.
- Minimally invasive
- Reversible and adjustable
- Life-enhancing potential
Deep Brain Stimulation (DBS)
Conditions Treated:
- Parkinson’s Disease – Reduces tremors, rigidity, bradykinesia, speech, gait & medication needs
- Dystonia – Helps control involuntary muscle contractions, postures like tilted neck, trunk or hand
- Epilepsy – Reduces seizure frequency and semiology in drug-resistant cases and reduces the seizure medications by 70%
- Chorea (e.g., Huntington’s Disease) – Manages abnormal involuntary movements there by improving the quality of life
- Alzheimer’s Disease – Helps in improving memory upto 40%
- Prolonged Coma (Disorders of Consciousness) – Potential to stimulate arousal and awareness in selected cases
- Obsessive-Compulsive Disorder (OCD) – Helps when medications & therapy fail – improves the obsession and compulsion and reduces the medications by 70-80%
- Depression, Schizophrenia and Bipolar disorder – Investigational but promising in treatment-resistant cases and reduces the psychiatric medicines by 70%.
- Addiction – helps the patient who are addicted to Alcohol, Narcotics etc..
- Obesity – helpful to the patients who are not improving with the conservative measures like diet control and exercise.
👨⚕️ “DBS can offer a new lease on life for patients struggling with conditions once considered untreatable.”
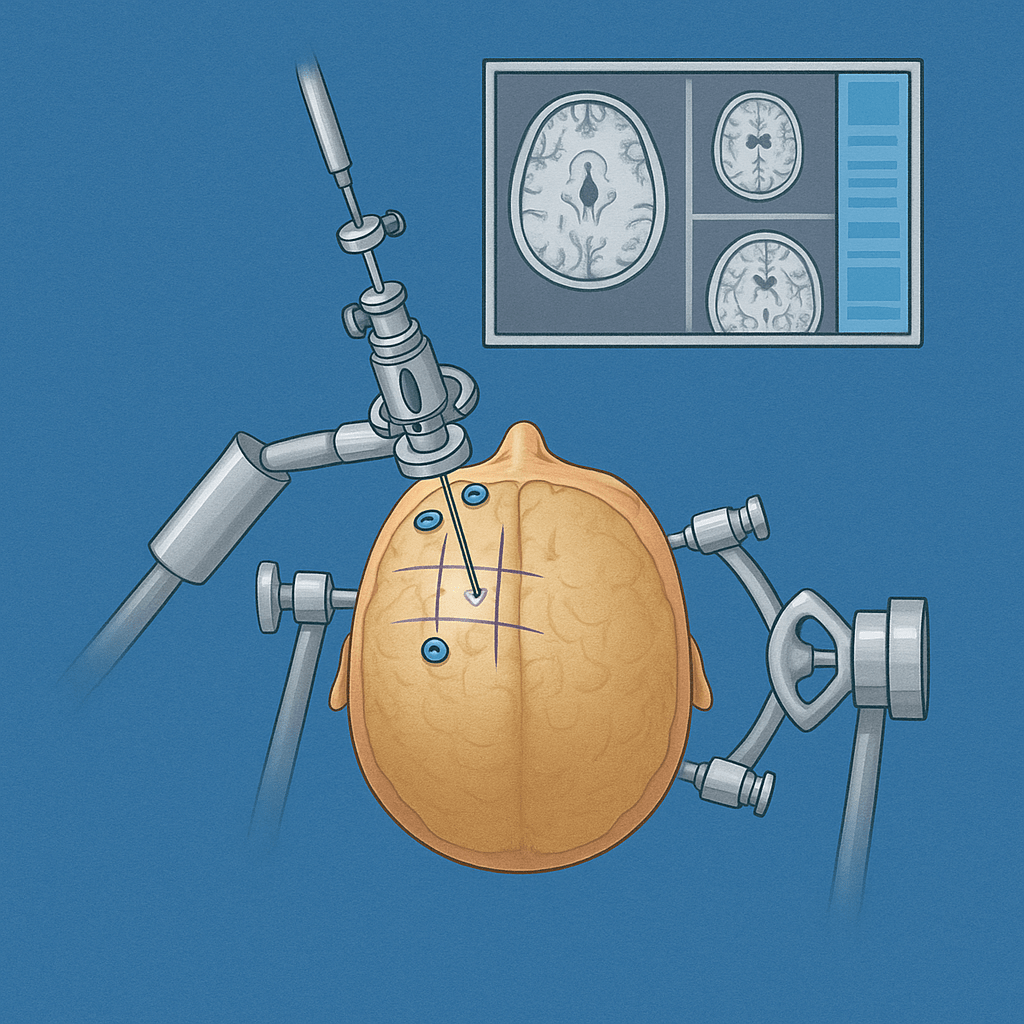
Procedure:
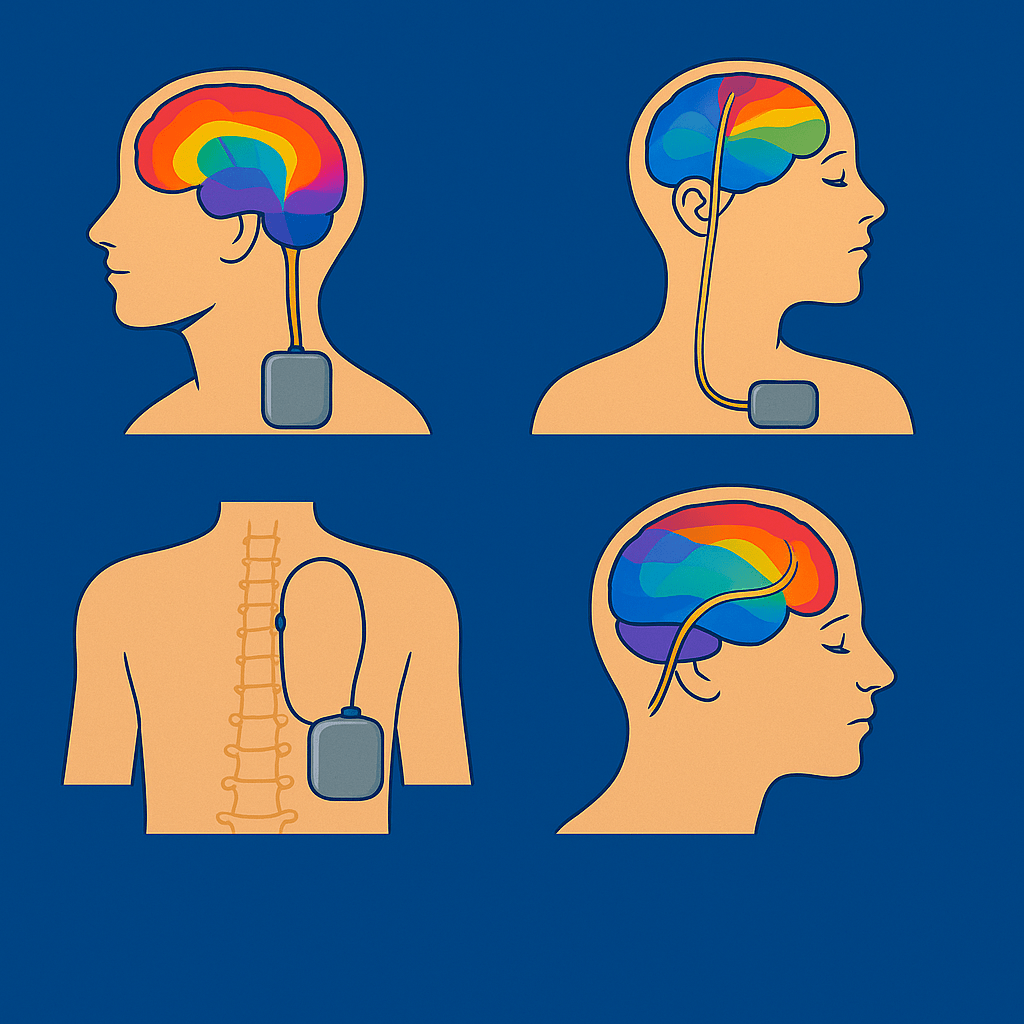
- Involves implanting electrodes into specific brain targets and connecting them to a pulse generator (pacemaker).
- The procedure is done by keeping the Parkinson’s patient awake
- High precision oriented and minimal invasive surgery
- Results are appreciated and checked by the Parkinson’s patient during the procedure
- Instant results on the operation table
- The procedure is completely reversible, no brain structures are burned, removed or cut.
- The treatment effect lasts for more than 15 years.
- No maintainence cost involved
- The entire implant is concealed and implanted inside the body, no wires are visible outside
- Immediate postop recovery and comfortably tolerated by elderly patients up to the age of 80.

Safety: Minimally invasive with well-established safety profile when performed by experienced teams.
Lesioning surgery
Used for: Tremors, Writer’s Cramp, focal dystonia, hemidystonia, Parkinson’s, Psychiatric disorders.
Procedure:
- Minimal Invasive key hole surgery done in awake condition. A thin wire is inserted into the circuit of the brain and a lesion is created with the help of RF generator.
- During the procedure the results are being appreciated by the patient and provides instant relief. Patient will be discharged next day morning.
Safety: Safe and cost-effective procedure with excellent results. It serves as an alternative procedure for the patients who cannot afford DBS.
Spinal cord stimulation (SCS)
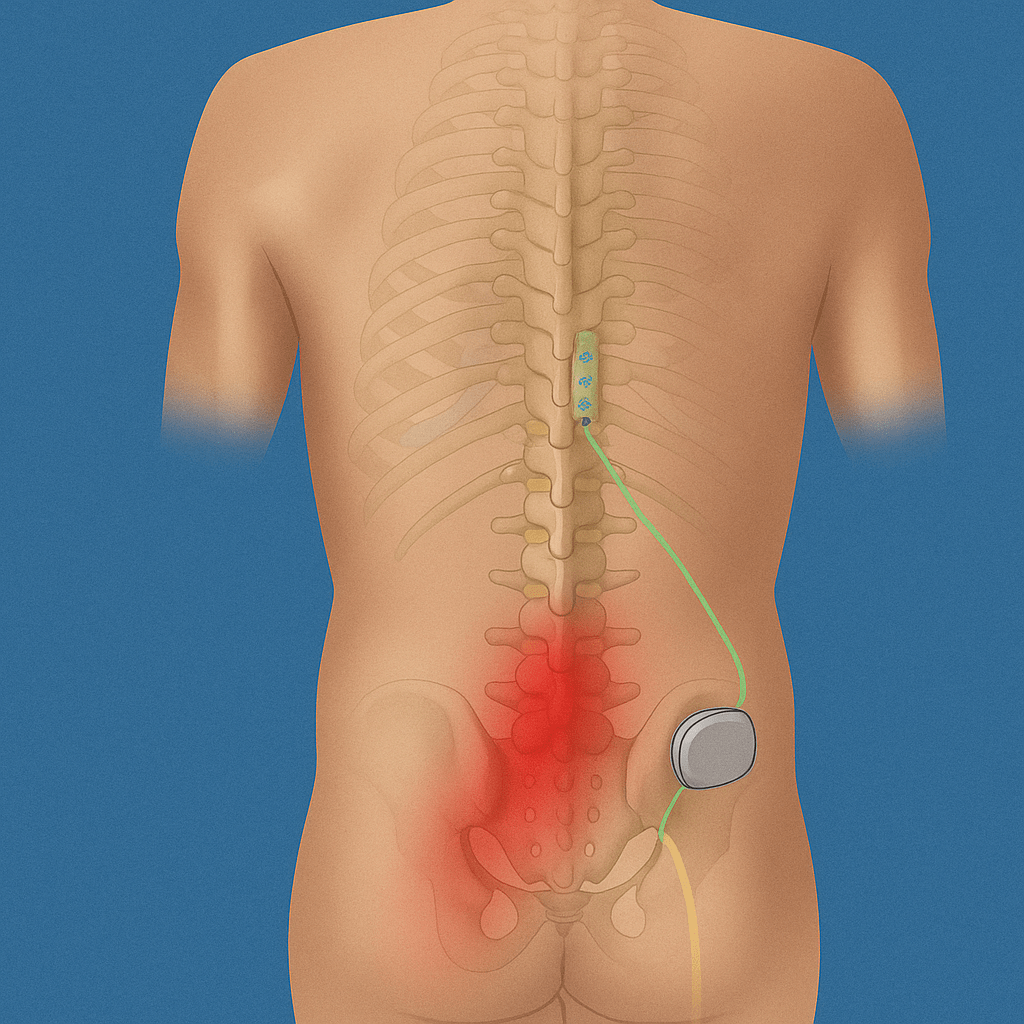
Used for: Chronic pain, Failed back surgery syndrome, Peripheral neuropathic pain, Onco-origin pain, SCI pain.
Procedure: Minimal-Invasive and involves placing electrodes in the spinal epidural space with a pulse generator implanted in the abdomen or back.
Safety: Safe and reversible procedure with adjustable therapy.
Motor cortex stimulation (MCS)
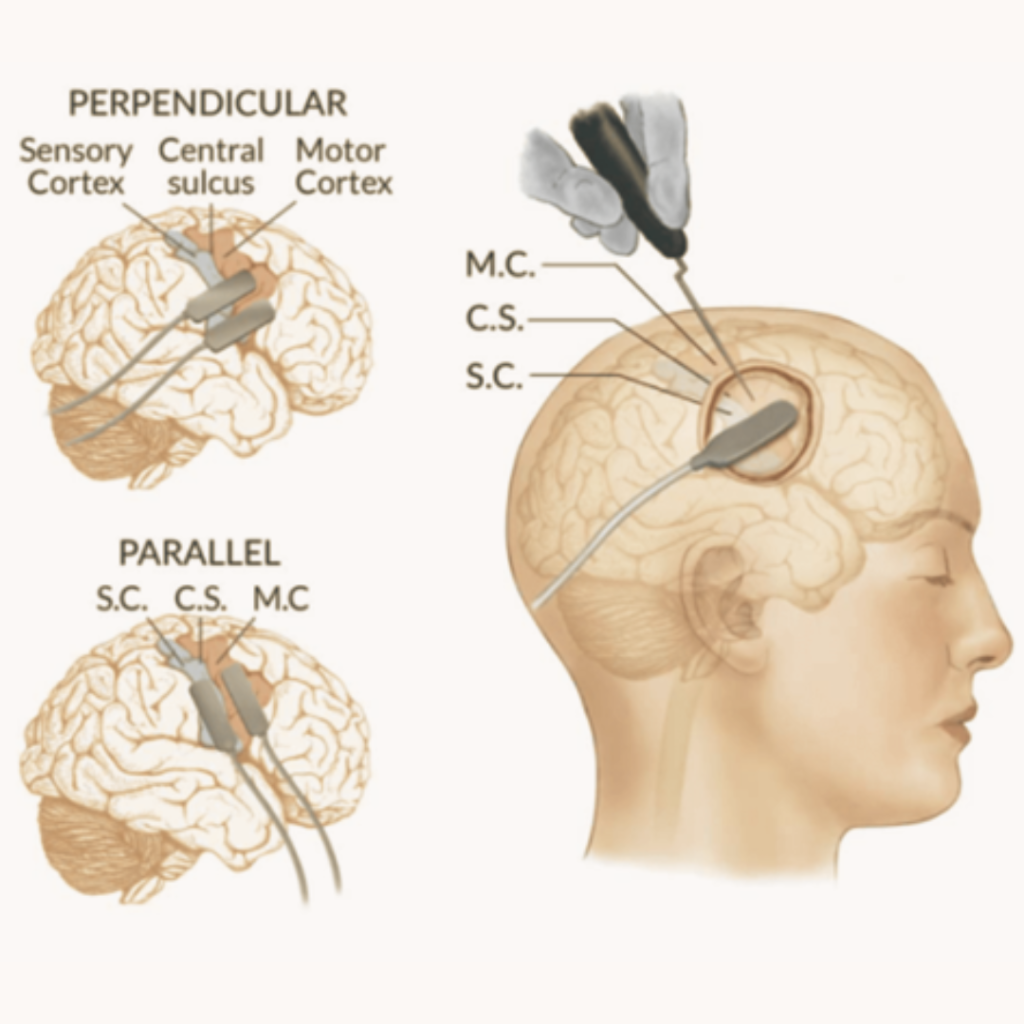
Used for: Epilepsy, Thalamic pain syndromes, residual Stroke-induced motor weakness not responded to physiotherapy and for thalamic pain syndrome cases.
Procedure: Electrodes are placed over the motor cortex through a mini-craniotomy and connected to a pacemaker placed in the chest.
Safety: Reserved for select cases; generally well-tolerated.
Sacral nerve stimulation (SNS)
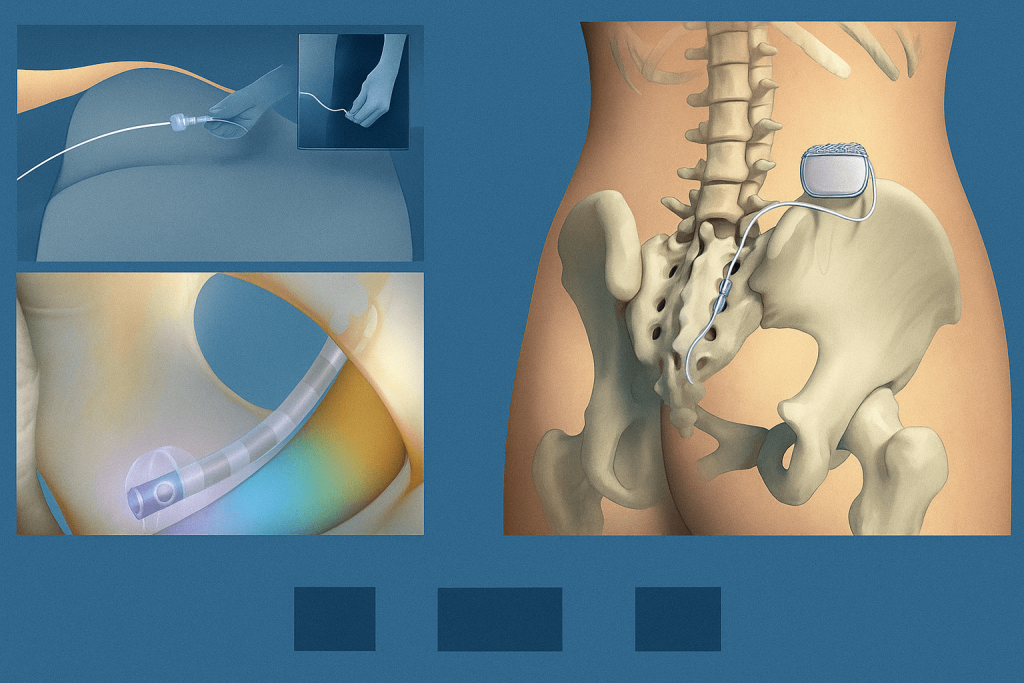
Used for: Urine and bowel incontinence, Urinary retention, urgency, hesitancy.
Procedure: A small wire device is implanted near the sacral nerve through an injection to improve bladder/bowel control. A trial electrode is placed and looked for three days for the improvement in the bladder control. If there is improvement then the permanent placement of the implant is done.
Safety: Outpatient procedure, low risk, effective in loss of urine and bowel control patients.
Phrenic nerve stimulation (PNS)
Used for: Ventilator-dependent patients (SCI, brain stem injury, CHS, GBS).
Procedure: Electrodes are implanted adjacent to the phrenic nerve on both sides of the neck to activate diaphragm contractions. In 6-8 weeks the patient will be able to breathe on his own and can be weaned off the ventilator.
Safety: Can reduce ventilator dependency; careful patient selection is critical.
Intrathecal Baclofen Pump Therapy
Used for: Intrathecal Baclofen Therapy (ITB) is a treatment method for severe spasticity. ITB uses a Intrathecal drug (baclofen) that is delivered into the cerebrospinal fluid around the spinal cord (intrathecal). It is helpful to improve spasticity in CP, SCI, TB spine, arachnoiditis, post-surgical cases.
Procedure: Minimal Invasive – A pump delivers baclofen directly into the spinal fluid. The drug is placed into an adjustable pump (baclofen pump) that is usually placed under the skin in abdominal area. The adjustable pump delivers baclofen to the Intrathecal area through a small tube (catheter). Since the pump is adjustable, we can titrate the dosage of baclofen externally through a remote.
A trial injection is given before the procedure to look for the tolerance and spasticity improvement before the actual implant fixation.
Lesioning Procedure
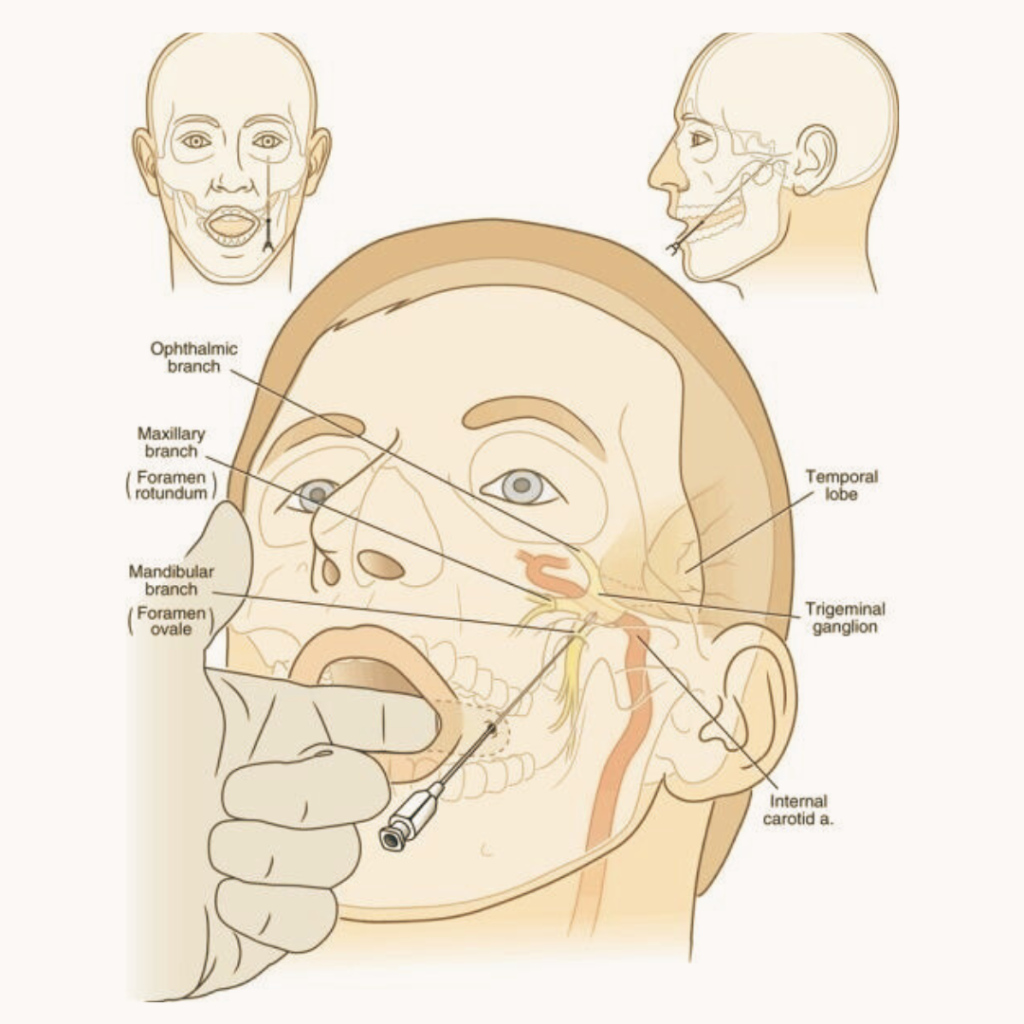
Used for: Trigeminal Neuralgia.
Procedure:
- RF lesioning – Minimal-invasive focused targeting of trigeminal nerve root ganglion.
Safety: No incision, Only injection near the angle of the mouth, day care procedure, minimal side effects.
- Cyber Knife: It is an incision less procedure in which the lesion is created with the beam of X-rays. The patient has to lie down on the Cyber knife machine and in 20 mins the procedure is completed. Patient can go home on the same day.
Used for – Various neurological disorders like trigeminal neuralgia, brain tumors, Psychiatric conditions and epilepsy.