Simple tips to protect your skin while wearing a mask

Wearing a mask for longer periods can lead to many skin issues. Make sure your skin is safe too with these easy tips One cannot avoid wearing a mask as it is one of the most potential measures to slow the spread of coronavirus, but wearing one can be harsh on your skin, especially if it is the sensitive type. Wearing masks for a longer period of time can invite skin irritation, bruises, or even breakouts. Here are a few essential tricks to take care of your skin while wearing a mask, said Dr Shraddha Deshpande, consultant plastic and reconstructive surgeon, Wockhardt Hospitals. Continuous use of masks allows oil and sweat to build up, traps your breath and creates a warm, humid environment leading to acne (breakouts), rashes, skin irritation, bruises, or skin infections. Following these tips can come handy to avoid such skin-related issues.
Elixir for your Knee arthritis – Knee Replacement by Advanced “Novo Technique” at Wockhardt Hospitals Nashik

We often hear words like arthritis, joint pain but do we have exact and accurate information about it? There is lot of misunderstanding about it in the society even today. Any joint pain we refer to as arthritis is completely wrong. The reality is that arthritis is not a disease, it is a result of our lifestyle. In the past, there was a time where osteoarthritis occurs only after age of fifty. But nowadays, due to hectic lifestyle, arthritis appears at younger to middle age. There are many types of it, among which most common is “Osteoarthritis”.(i.e. age related wear and tear of joint.) Between two bones of each joint is a layer of cartilage, it’s the cushion between two bones. This layer of cartilage prevents friction between the two bones and facilitates movement of the joint. Over time, the cartilage layer rubs off, causing the bones in the joints to rub against each other which becomes painful swollen n deformed, this condition is referred as “osteoarthritis” in medical science. This condition is more common in the knee joint in Indian population as we follow cross legged sitting and use Indian type of toilets which results in more wear and tear. In today’s fast-paced world, lifestyle changes such as eating and drinking habits, obesity and even some biological factors are responsible for this. Common symptoms of osteoarthritis include knee pain after walking, swelling/inflammation in knee, inability to turn legs, bending legs, and consequently inability to walk. Osteoarthritis causes a lot of pain and slows down the movement of the joints, resulting in reduced quality of life and you won’t be able to carry out daily activities, e.g. Walking, kneeling, exercising, climbing stairs, playing with grandchildren, etc. The most important factor in the treatment of osteoarthritis is to classify it. With the help of X-ray or MRI, the wear and tear of the joint is usually classified in four stages. Osteoarthritis of stage 1 and 2 is treated with medication and certain exercises. But when medication and exercise doesn’t help and osteoarthritis is in stage 3 or 4, having Total Knee Replacement (TKR) Surgery is a best option available. In a joint replacement surgery both bones of the joint are given a specific shape for an implant to be fixed which is made of a special metal, a layer of plastic is placed between two implants to compensate the cartilage and to stop the friction of the implant. In this surgery, no muscle or ligament is cut near the joint. This surgery relieves the pain and allows the patient to live a normal life. At Wockhardt Hospitals, Nashik, Total Knee Replacement (TKR) Surgery is performed in a special and unique way called as “Novo Technique”. Surgery with this method reduces the incision on the skin, reduces the time required for the operation, reduces bleeding, eliminates pain, reduces the need for physiotherapy, and speeds up the recovery. Novo technique almost assures 100% satisfaction to patients after surgery. After implantation, ease of movement of joints increases and quality of life improves. Furthermore, in today’s fast-paced world, we do not have to be dependent on others to take care of ourselves. After this surgery, patients can do all the daily activities, they can climb stairs, sit crossed legged, exercise and even sit on Indian form of commode. In view of all this, I would like to tell everyone not to bear the pain of osteoarthritis, timely treatment can make rest of your life more comfortable, all you need to do is seek medical guidance at the right time. Dr. Jayesh SonajeMBBS, MS (Ortho), Fellowship in Joint Replacement & Arthroscopy (Germany)Consultant – Joint Replacement & Orthopedic SurgeriesWockhardt Hospitals Nashik For Appointment, Call – 02536624444
Turn to nutmeg aka jaiphal to kickstart your weight loss journey in no time

Spices are known to catalyze your metabolic activity, and that’s why nutmeg works wonders for weight loss. Read on to know more. Of course, you can work out hard in the gym to lose that stubborn fat, but what if we tell you about a miracle spice that can accelerate weight loss? Yes, if quick and sustainable weight loss is on your mind, then it’s time to raid your kitchen for nutmeg aka jaiphal. Since time immemorial, nutmeg has been used for medicinal purposes. And when it comes to your gut, this spice is all you need to keep it in top shape. That means your digestion and metabolism will also be on track. Everything put together will lead to weight loss. Amreen Shaikh, a dietitian and nutritionist from Wockhardt Hospital, Mumbai, suggests that a little less than half a teaspoon or a pinch of nutmeg powder every alternate day can be your tonic for weight loss. 1. Nutmeg eliminates toxins from your body, and has digestive properties that can help in increasing metabolism, thereby helping with weight loss. 2. It is also known to suppress appetite, because it is rich in fibre. That means no more unwanted binge sessions, which are the real cause of weight gain. 3. Jaiphal helps in fat burn. Yes, this amazing spice contains some essential minerals, and one of them is manganese which helps to break down fats. 4. Nutmeg helps you sleep. Did you know, lack of proper sleep can also lead to weight gain? In case sleepless nights are a cause for trouble, then try nutmeg. “Nutmeg is great when it comes to the treatment of insomnia or sleeplessness in general. Sleeping better aids in weight loss. You can drink a glass of herbal tea with nutmeg powder to induce a good night’s sleep,” she suggests. 5. Nutmeg is a good antidote for stress. Stress is also a factor that needs to be kept in check if you want to lose weight. “Thanks to antioxidants present in nutmeg, it helps in the prevention of oxidative stress in cells. When cells are suffering from oxidative stress, it leads to obesity,” she explains. “Please keep a check on the quantity of nutmeg you are consuming, because you can only get all these benefits if you have it in moderation,” says Ms Shaikh. The bottom line Without a doubt, nutmeg is the ultimate wonder spice. Not just weight loss, but nutmeg also helps in dealing with disorders like diabetes, arthritis, etc. But if you are pregnant or allergic to it, then you should stay away from nutmeg. You can add nutmeg powder to soups, green teas, dal, etc, as consuming it as it is is not the best option. It’s pretty bitter to taste! So ladies, go nuts for nutmeg and give your weight loss regimen a little push. Source: https://www.healthshots.com/healthy-eating/superfoods/heres-how-you-can-use-nutmeg-for-weight-loss/
Successful Brain tumor resection surgery on a 72-year-old septuagenarian

A septuagenarian with a large pituitary tumor underwent safe endoscopic endonasal surgery at Wockhardt Hospitals A team headed by Dr. Mazda Turel, Neurosurgeon, Wockhardt Hospitals, South Bombay, along with ENT specialist Dr. Neepa Vellimutam successfully performed a complicated brain tumor resection surgery on a 72-year-old septuagenarian from Mumbai who was brought with a progressive vision loss. It was revealed that the patient was diagnosed with 4 cm pituitary adenoma pressing on his optic nerve causing blindness. A timely intervention by the neuro-oncology department gave him a fresh lease of life. He has been discharged last month with no complications. Dhansukhlal Dedhia, a resident of Mumbai developed prostate cancer earlier this year for which he underwent Transurethral resection of the prostate (TURP) in May 2020 and was on chemotherapy and steroids. Life was smooth but a few months ago, he started encountering vision problems and that took a toll on his active life. The patient was dependent on his family members for carrying out his daily chores. However, his health deteriorated further and he was referred to Wockhardt Hospitals, South Bombay. Dr. Mazda Turel, Neurosurgeon, Wockhardt Hospitals, South Bombay said, “On September 8, 2020, the patient presented with the history of bilateral blurred vision for the last few months. His vision deteriorated over days and was unable to see things beyond afoot. The MRI showed a 4cm tumor pressing against the optic nerves causing visual loss.” The oncologist collaborated that prostate cancer was under control and it would be worth going ahead with surgery to restore vision. Dr. Turel added, “The patient was scheduled to undergo endoscopic endonasal tumor resection. His COVID test done a day prior to surgery was negative. The patient underwent Endoscopic transnasal trans-sphenoidal radical excision of pituitary macroadenoma under general anesthesia on September 9, 2020. An endoscope with light and camera was inserted in one nostril and advancing it to the back of the nasal cavity. A small portion of the nasal septum that divides the left and right nostril is removed. At the back wall of the sphenoid sinus, there is the bone overlying the pituitary gland known as the sella, and is removed to expose the tough lining of the skull called the dura. The dura is opened to expose the tumor and pituitary gland and the tumor is extracted. Tumor removal corrects vision problems and restores normal hormone balance. He had also developed transient hyponatremia which was corrected Dr. Turel explained, “We removed the tumor completely relieving the pressure from his optic nerves. He made a good recovery and was back to reading the newspaper within 4 days of surgery. He was discharged with near-normal vision.” “This surgery is particularly challenging in times of Covid given that the nasal passage is a harbinger of infection and operating through the nose and drilling the base of the skull generates aerosols. The level of precaution even in Covid negative patients is extremely heightened since the entire operation theatre is at great risk of receiving or transmitting the infection from an asymptomatic person.” “I was disheartened when I had blurred vision and was not able to recognize who was standing in front of me as I couldn’t see. My vision problems were going on increasing as the days passed. Fortunately, Wockhardt Hospitals came to my rescue. I thank the doctors for helping me gain my vision back and giving me a new way of life,” concluded patient Dhansukhlal Dedhia.
Are you Having Arthritis? Know About the Treatment Options to Tackle it

Rheumatoid arthritis treatment options: Arthritis is a bothersome condition and can also take a toll on one’s mental well-being. Arthritis diseases can damage joints very quickly, and arthritis may be a part of a more severe disease affecting multiple organs of the body. Today, we tell you what arthritis and advice to tackle it appropriately is. Arthritis means joint pain with some signs of inflammation like swelling, redness, stiffness, and decreased range of motion. Arthritis or arthritis diseases can be of more than 20 types, and different types are managed differently. Arthritis diseases can be very complex and do not necessarily affect older adults. The most common arthritis we see in the general population is Osteoarthritis (OA). Osteoarthritis usually occurs with increasing age and age-related joint wear and tear play a significant role in the occurrence of this type of arthritis. Osteoarthritis tends to affect one’s hands, knee, hip, and spine. Hence, it is necessary to know which type of arthritis disease one suffers from. If you Have Arthritis-like Symptoms, the Following Things Can Be Done to Seek Adequate Relief Diet: There are a lot of myths and misconceptions about diet for arthritis patients. Always clear your myths with an arthritis expert like a Rheumatologist. The old-age Indian mythology that sour (that food) like tomato, curd, lemon, oranges, tamarind, etc., and other foods like chana dal, cabbage, rice, non-vegetarian food, etc. because arthritis is not based on any substantial evidence. The concept that all arthritis is related to uric acid is also wrong. Foods like oranges, guava, etc. provide vitamin C, which is very good for general health. Chana dal, low-fat dairy products, etc. can provide proteins essential to build muscle strength in arthritis patients. In short, the best dietary advice is to eat what suits you and eating a healthy and balanced diet most times. Exercises: Physiotherapy or some form of activities may be advised to help you strengthen your joints and increase mobility. Strengthening your joints and reducing stiffness is essential. You can opt for walking, cycling, aerobics, and even swimming which can be beneficial for your joints. You can even do cardio and strength training under guidance. Always consult your doctor for appropriate exercises. Surgery: Surgery is an option if the joint is severely damaged. Hip, knee, or other joint replacement surgeries can be done in selected patients. These surgeries can be beneficial in restoring mobility and function in patients with persistent pain, limited mobility, and advanced joint damage. A rheumatologist is a physician who can diagnose different types of arthritis or similar diseases and also determine their severity. If one has significant joint pain, they should strongly consider seeing a Rheumatologist. The rheumatologist will evaluate the patient and form a plan based on severity. They may advise taking medications to reduce pain, swelling, and inflammation of joints or other organs. Disease-modifying antirheumatic drugs (DMARDs) may be given to modify or control your disease. DMARD’s can help to prevent joint or organ damage.
Rare Neurological Disorder, Guillain-Barré Syndrome, Linked To COVID-19 successfully treated at Wockhardt Hospitals, South Bombay

37-year-old Ms. Jyotsna Maru was diagnosed with Guillain-Barré syndrome after suffering from Covid-19. It is an autoimmune disease which results in paralysis of limbs due to delays in sending signals through the nerves. Several reports of covid 19 associated GBS have been reported from different parts of the world and India. She was successfully managed by Wockhardt Hospital South Bombay critical care team lead by Dr. Kedar Toraskar, Chief of Critical Care, Dr. Ravindra Zore, Dr. Gaurav Gupta, Dr. Bhooshan Gondse and Dr. Gurudas Pundpal with Dr. Prashant Makhija, Consultant Neurologist and Dr. Honey Savla, Junior Consultant. A Youtuber and Bharatanatyam Dancer Ms. Jyotsna Maru visited Wockhardt Hospitals with the complaints of tingling, numbness involving hands and legs along with progressively worsening weakness which worsened to the extent that she was unable to stand and walk on her own. She tested positive for Covid-19 infection. During Hospital stay for COVID treatment Ms. Jyotsna had complaints of severe backache and difficulty in walking. In view of progressive weakness, she was suspected to have Guillain barre syndrome, which was confirmed on neurological evaluation. Dr. Prashant Makhija, Neurologist Consultant, Wockhardt Hospitals, South Bombay said, “Guillain Barre Syndrome (GBS) is an autoimmune disorder in which our body’s immune system goes in overdrive and starts mistakenly attacking nerves of our hands and legs, leading to paralysis of limbs. It usually appears days or weeks after a viral infection which is usually a respiratory or gastrointestinal infection. In her case, COVID-19 infection might have led to Guillain-Barre Syndrome. With appropriate treatment, she has now significantly recovered and is able to walk with minimal support.” Dr. Kedar Toraskar, Chief of Critical Care, Wockhardt Hospitals South Bombay said “Several reports of Covid-19 associated GBS have been reported from different parts of World and India. It a rare neurological complication which is associated with COVID 19 virus and which can be potentially life-threatening and may require mechanical ventilatory support. If diagnosed and treated on time with Intravenous immunoglobulin (IV IGg) or plasmapheresis, life-threatening complications can be averted. This is a rare neurological complication that can lead to respiratory failure and even death. But if diagnosed and treated early like Ms Jyotsna the outcomes are good.” “Due to numbness over my fingers, difficulty in walking, and severe backache, I was really worried about my health and my career. I feared whether I will be able to perform Bharatanatyam. I am glad about timely treatment, I am recovering well. I sincerely thank the team of doctors at the Wockhardt Hospitals who always motivated me and supported me with proper care and treatment. I am thankful to the doctors for helping me recover and hopefully, I will be able to perform Bharatanatyam very soon.,” concluded patient Ms. Jyotsna. Source: http://mediabulletins.com/health/rare-neurological-disorder-guillain-barre-syndrome-linked-to-covid-19-successfully-treated-at-wockhardt-hospital-south-bombay/
When There Is A Volcano In The Head

Migraines are very common, and democratic, affecting the poor and famous alike but can be tackled with medication and lifestyle change. “I need you to help me with this headache I’ve had for a decade,” a friend pleaded. “As long as you’re not referring to your boss, I’m happy to try!” I shot back. He was my age, only better looking and with more hair. In his mid-twenties, he’d started developing a peculiar throbbing pain on the right side of his head. It was typically associated with a few zig-zag shadows he perceived before the headaches heightened. Lights and sounds worsened the discomfort, and he’d prefer a dark, cool environment during an attack. “When I massage that part, the ache mysteriously scrams to another part of the head, never really going away,” he said, describing his dilemma. “The nausea is so severe, I need to force myself to vomit, often half a dozen times, shoving fingers down my throat to induce the last remaining bits in my stomach to be expelled. It is only when my stomach is absolutely empty that the throbbing headache finally eases. Then I gargle, have a sip of water, and sleep it off, waking up only several hours later.” His medical test reports were unblemished and his scans spotless. Yet, over time, his migraine worsened in frequency and intensity, from once in three months to every three days and lasting the entire day. He promiscuously popped pills, but reached out to me only when he realised he was hanging on to the end of a burning rope and needed someone to douse the fire. “One can get a headache from taking too many headache pills,” I cautioned. “It’s called MOH or medication overuse headache,” I smiled, bemused by this obvious paradox. “Isn’t there any surgery for this stuff? Sometimes I feel as if cutting my head open will relieve the pain.” I went on to explain that in ancient Greece, headaches were considered powerful afflictions. Victims prayed for relief from Asclepius, the god of medicine. If the pain continued, a medical practitioner would drill a small hole in the skull (trephination) to drain the confined demons. Unfortunately, this dire technique often replaced the headache with a more permanent condition. And, to relieve that, they applied raw potatoes, cabbage, and onions to the head. Some deeper medical insight into the anatomy and physiology of the pain producing structures in the cranium have led us to understand that migraines involve alterations in the subcortical sensory modulatory systems that influence the brain widely. “Whatever that means,” he flared up, confused, wanting to simply rid himself of the periodic curse. “Just like your zig-zag lines, the distortion of perceptions described in the famous 1865 novel Alice’s Adventures in Wonderland is believed to have stemmed from Lewis Carroll’s own experiences with episodes of micropsia (the visual perception of objects appearing smaller) and the constitutional auras resulting from his migraines,” I said, thinking I’d lighten up the conversation with some trivia. Patients are almost instantly relieved when they know that someone famous suffered from the exact same ailment as them. Darwin, Nietzsche, Freud, Caesar, Napoleon, Van Gogh, Picasso, Thomas Jefferson, Virginia Woolf, and Elizabeth Taylor were all famous migraineurs. “I’d rather feel nothing than feel the pain I’m feeling,” revealed Elvis Presley, resorting to gargantuan amounts of drugs to battle chronic headaches, an overdose of which was speculated to be the cause of his death. Neurologists call this distortion of perception that precedes the migraine headache, the Alice in Wonderland syndrome, and they think it’s due to an abnormal amount of electrical activity that results in excessive blood flow to parts of the brain that process visual perception and texture; I wonder what JK Rowling went through when she wrote the Harry Potter series! Migraine needs to be treated medically with a two-pronged approach of medication and lifestyle modifications. The medication I prescribed was a combination of prophylactic and abortive therapy to be taken for three months; the prior to be consumed daily and the latter just before an attack. In addition, one is expected to sleep adequately and eat in moderation, avoiding chocolate, cheese, coffee, and wine—all circumspect triggers for migraine. “Why does everything enjoyable have to be linked to a price you pay?” my friend lamented. “A migraine ‘shot’ is also available now, which you can take once a month to dampen symptoms,” I added, “but we’ll keep that for later.” I also asked him to maintain a headache diary with monastic ferocity to document the vivid details of his auras and time periods of each attack in relation to the medication, in an attempt to analyse how to alter treatment, if required. He also needed to document his sleep timings, travel habits, and foods that triggered his headaches. Various forms of neuromodulation such as transcranial magnetic stimulation and non-invasive vagal nerve stimulation have also been attempted when medication alone does not suffice. Modern surgery involves trigger point deactivation, which essentially involves transecting or blocking a sensory nerve responsible for the affliction, which, like all surgery, comes with its risks. My friend returned three months later, regaining full control of his life. Now, he worries only about an occasional, easily manageable headache: no auras, no vomiting, not skipping important life events. He was well, but I noticed that he wasn’t beaming. “You’re more than 99 per cent better and we managed that without drilling a hole in your head!” I exclaimed. “Why aren’t you more delighted?” He replied, “I can’t blame my boss for everything anymore!” Source: https://www.mid-day.com/articles/when-there-is-a-volcano-in-the-head/23090258
Struggling with PCOS? Try these workouts to manage the syndrome better
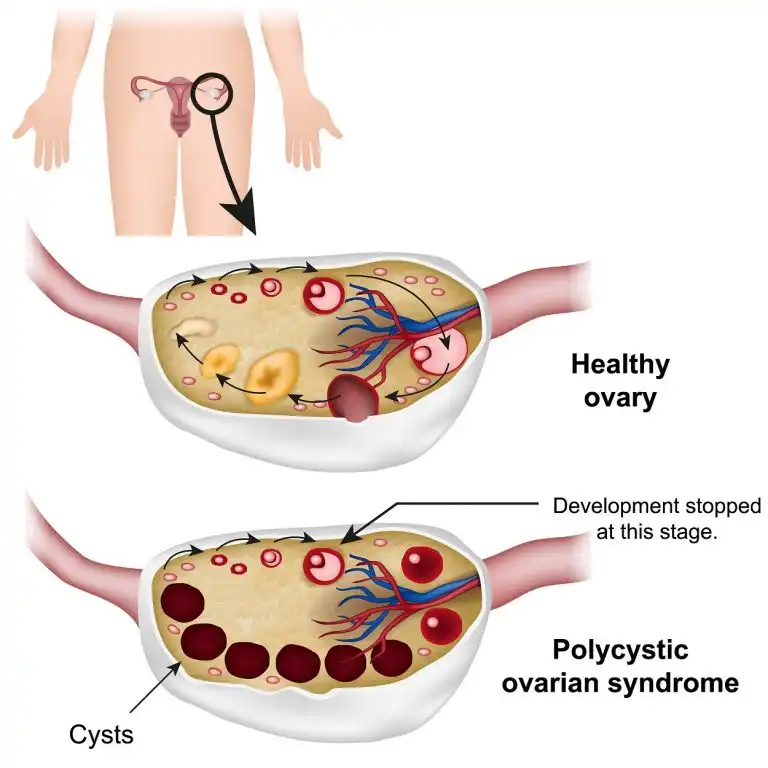
PCOS or polycystic ovarian syndrome can cause various issues but it can also be managed with regular workouts. These 4 exercises can help you in a big way! If you suffer from the polycystic ovarian syndrome, you already know how physically and emotionally distressing it can be. It is a hormonal condition that can cause multiple issues but one of the most prominent ones is weight gain. Apart from weight gain, PCOS wreaks havoc on your body in several other ways. Your body produces testosterone in higher quantities which can cause some major changes in your menstrual cycle. It also leads to reduced fertility, increased hair growth, and changes in your skin such as acne or darkened skin patches. In most cases, it also causes insulin resistance. PCOS affects up to 18 percent of women but can be managed with a nutritious diet and regular physical activity. So, let’s take a look at the 4 workouts you need to get to for PCOS. All set? 1. Cardio Try and include moderate exercises like brisk walking, jogging, cycling or swimming to help tackle symptoms of PCOS. These exercises increase your body’s response to insulin, reducing the risk of cardiovascular diseases and type 2 diabetes. Take out 30 minutes every day for cardio. You’ll definitely see a change in your weight and mental health. 2. Strength training It’s extremely helpful in reducing insulin resistance and increasing the metabolism rate. Make sure you include strength training as part of your fitness regimen. You can try bodyweight exercises like squats, push-ups, or tricep dips to improve the function of insulin in your body. What’s more, it can also accelerate your metabolism by building more muscle mass. If you combine resistance moves with cardio, you can get a lean body. Now, isn’t that absolutely amazing? 3. High-intensity interval training It’s really not about exercising for too long but doing it the right way. Hence, it is important to swap between short bouts of high-intensity exercise and low-intensity recovery. Not only does it boost your cardiovascular fitness, but it also benefits those with PCOS. Exercise on a spin bike for only 10 to15 minutes and burn calories while reducing abdominal fat more effectively. 4. Core strength If your weight is above the normal range, you can suffer from severe back pain and poor posture. Hence, including core training in your fitness routine is important. These muscles support your spine and must be strengthened. If you are trying to conceive, make sure to also train your pelvic floor muscles. They’re a vital part of your core, helping tackle urinary incontinence, boosting sexual health, and enhancing pelvic stability. Ladies, it’s time to focus on your fitness regime, and reduce the symptoms of PCOS! Source: https://www.healthshots.com/fitness/staying-fit/pcos-and-exercise-4-workouts-to-try-if-you-have-pcos/
Covid-19 positive pregnant woman gives birth prematurely at Mira Road hospital, mother and baby discharged

A 35-year-old woman from Mira Road beat Covid-19 and went on to successfully deliver her baby in the 7th month of her pregnancy. Both the mother and baby were discharged after the woman spent 60 days in the hospital, including 21 days in the intensive care unit (ICU) and 14 days on the ventilator. The patient was referred to Wockhardt Hospitals in Mira Road, after she complained of fever, breathless and desaturation (low blood oxygen concentration), said Dr Bipin Jibkhate, a senior critical care consultant at the hospital. “The patient was taken to a private practitioner, and after testing positive for Covid-19, she was shifted to our hospital. There were multiple challenges in managing the pregnant patient in the ICU as her immunity was low. Her physiological needs were different from normal women, and pregnant women have a higher tendency of clotting, high abdominal pressure, low carbon dioxide levels and higher tendency to vomit, said the medico. In such situations, if the oxygen level is not maintained, the options are limited, Dr Jibkhate explaining, adding that they had to put the patient on the ventilator. “Fortunately, she responded to the treatment, and her ventilator requirement went down. However, even after seven days, she required a significant amount of ventilator use, and so we removed the tube from her mouth and put it through her throat – a procedure called as tracheostomy,” he said. In the meanwhile, the woman’s second Covid-19 test came negative. She was shifted to a non-Covid ICU and slowly taken off the ventilator. “Because of the stress of the disease and ICU stay, the patient went into labour prematurely and delivered a baby boy,” said Dr Mangala Patil, obstetrician, Wockhardt Hospitals. According to Dr Samir Shaikh, consultant neonatologist, the baby weighed only 1,560 gram and was shifted to the neonatal intensive care unit (NICU). After a few days, the baby’s condition improved, and he and his mother were discharged. “My world came crashing down when I tested positive for Covid-19. But the doctors made sure that I delivered my baby safely, and now his health has also improved,” said the patient. Source: https://www.hindustantimes.com/cities/covid-19-positive-pregnant-woman-gives-birth-prematurely-at-mira-road-hospital-mother-and-baby-discharged/story-Yc3lm2JUtnaxQ7RD5NhqTO.html
Why Some People Are More Sensitive Than Others?

A highly sensitive person (HSP) is a term for those who are thought to have increased or deeper central nervous system sensitivity to physical, emotional, or social stimuli Are you a highly sensitive person? or Do you know someone in your personal or professional life who are highly sensitive? Well, High sensitivity can be defined as acute mental, physical, and emotional responses to external (social, environmental) or internal (intra-personal) stimuli. A highly sensitive person can be an introvert, an extrovert, or somewhere in between. A highly sensitive person (HSP) is a term for those who are thought to have increased or deeper central nervous system sensitivity to physical, emotional, or social stimuli. Some refer to this as having sensory processing sensitivity or SPS as a short form. Though there are many positive aspects of being a sensitive person like a greater ability to listen and having a greater empathy or intuitiveness and better understanding of others but high sensitivity also adversely affects one’s health, happiness, and success, and often complicates relationships. According to Dr. Sonal Anand who is a Psychiatrist in Wockhardt Hospital at Mira Road, Mumbai, Being highly sensitive can be a combination of your genetics and the environmental factors that play a big role. Like if you have a parent who is quite sensitive, the chances of you getting sensitive increases. It also depends on the kind of person that you have become like the experiences that you get or how you are brought up and the values you have learned can determine the sensitivity in you. By the age of 17 to 18, 95% of your personality is developed. “Well, being sensitive for few things is fine, like regarding your partner or spouse or relationship and family member as it can make your relationship better but sometimes being overly sensitive can lead to anxiety disorders and depression. This is the most common cause of depression, most of my patients who are in depression often say that they are very sensitive or little things upsets them a lot,” she said. “If feel that you can’t handle a situation or you are having anxiety or you are into depression, then you must visit your therapist for help. However, self-care and building your confidence matters a lot, while taking therapies can help you too. Moreover, self-help can be great for you, like you can identify which things make you more disturbed and you can work on it,” she added. While many people may experience some of these signs from time to time, a highly sensitive person will likely “feel too much” and “feel too deep.” Some individuals may be highly sensitive to just one or two stimuli, while others may be strongly affected by more on the list. Highly sensitive people are most of the times are described as being “too sensitive” and it is considered as a personality trait in people. These terms were first coined by psychologists Elaine Aron and Arthur Aron in the mid-1990s and interest in the concept has continued to grow tremendously since then. Anyone could be an HSP, whether a man or woman, adult or child. A high sensitive person has a more sensitive central nervous system, making them highly attuned to physical, emotional, or social stimuli than others. How Do You Know? High sensitivity is a personality trait that involves increased responsiveness to both positive and negative influence. But it is important to remember that being an HSP does not mean that you have a diagnosable condition. This applies to a few different categories There are several traits or characteristics common to HSPs, according to the researchers who identified this personality trait: However, HSPs experience higher levels of stress than others, and research has found they are also more prone to burnouts because they get easily overwhelmed. While, the lack of awareness of the trait can make dealing with hypersensitivity challenging for a lot of HSPs.