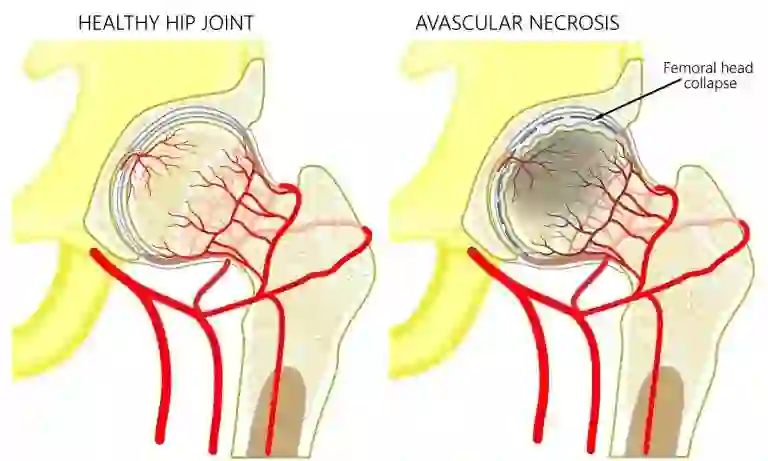
Avascular necrosis (AVN) of the femoral head, commonly known as osteonecrosis, is a condition that affects the hip joint, primarily impacting the blood supply to the bone. Left untreated, it can lead to pain, disability, and even the need for orthopedic treatment. As an orthopedic surgeon at Wockhardt Hospital, Mumbai Central, I believe in empowering patients with the knowledge to make informed decisions about their health. In this article, we will explore the stages of AVN and discuss the importance of seeking timely treatment. Additionally, we will shed light on the Direct Anterior Approach to hip replacement, a cutting-edge surgical alternative that offers early functional recovery for individuals dealing with this condition.
What is Avascular Necrosis?
The death of bone tissue as a result of inadequate blood flow is known as avascular necrosis. It is also referred to as ‘osteonecrosis’, and it can produce small fractures in the bone, eventually causing it to break down. The interruption or lack of blood supply causes bone tissue to break down, often resulting in pain, restricted movement, and, in severe cases, collapse of the affected bone. Commonly affecting the hip, knee, shoulder, and other joints, it can be triggered by injury, excessive alcohol consumption, steroid use, or underlying medical conditions. Anybody can get impacted. However, individuals between the ages of 30 and 50 are more likely to suffer from this condition. Early detection through imaging tests and timely intervention, such as medication, physical therapy, or surgery, is crucial to manage symptoms and prevent further damage.
Symptoms of Avascular Necrosis Femoral Head
Depending on the stage and the damaged bone, AVN symptoms might vary. Some individuals with avascular necrosis have no symptoms at all in the initial phases. As the condition worsens, the affected joints might hurt only when you put weight on them. After a while, the pain could even be too much to handle when you’re resting. Typical indications consist of:
- Persistent discomfort in the affected joint is often the earliest symptom. It may start mildly and worsen over time, limiting movement and impacting daily activities.
- Stiffness or reduced flexibility in the joint can develop gradually, making it challenging to perform regular movements.
- As AVN advances, the pain might become more intense and begin to radiate from the affected area to surrounding regions.
- Avascular necrosis in weight-bearing joints, such as the hip or knee, can make it challenging to stand, walk, or bear weight on the affected limb.
- Over time, due to limited use of the affected joint, muscles surrounding the area might weaken and shrink.
- In severe cases where AVN progresses without intervention, the bone structure may collapse, causing severe pain and severe limitations in movement.
Causes of Avascular Necrosis Femoral Head
Avascular necrosis is brought on by diseases or bone fractures that obstruct blood supply to bone tissue. Avascular necrosis can result from a number of disorders or treatments, including:
- Trauma or Injury: Joint dislocation, fractures, or direct trauma can damage blood vessels, hindering the flow of blood to the affected bone.
- Use of Steroid: Prolonged or high-dose steroid medications, often used to treat conditions like asthma, arthritis, or autoimmune disorders, can increase the risk of AVN by affecting blood vessel health and function.
- Excessive Alcohol Consumption: Heavy alcohol intake can weaken bones and affect blood circulation, particularly in the hip, leading to AVN.
- Medical Treatment: Cancer radiation treatment can deteriorate bone structure. Organ transplants, such as kidney transplants, are among the other disorders associated with AVN.
- Bisphosphonates: These bone-density-promoting drugs may cause mandibular osteonecrosis. If you’re taking them for metastatic breast cancer or multiple myeloma, this may be more likely to happen.
Nontraumatic AVN is also linked to the following conditions:
- Decompression sickness, which causes gas bubbles in your blood
- Diabetes
- HIV
- Gaucher ailments, in which a fatty material accumulates in the organs
- Inflammation of the pancreas, Pancreatitis
- Radiation therapy or chemotherapy
- Sickle cell disease
Treatment of Avascular Necrosis Femoral Head
The extent of damage in the bones will determine the course of treatment. Enhancing function and preventing more bone or joint deterioration are the two main objectives of therapy. If the extent of your bone deterioration is restricted to smaller, non-weight-bearing bones, your doctor may consider the following treatments:
- NSAIDs, or nonsteroidal anti-inflammatory medicines, are medications that help control pain and inflammation.
- Cold packs.
- Heat treatment.
- Rest.
- The joint function can be preserved or restored with physical therapy. Exercises targeted at enhancing muscular strength, lowering stress on the injured joint, and increasing joint mobility may be helpful.
- Walking assistance like crutches and canes.
Patients with more severe cases of avascular necrosis may require surgery to treat their conditions. Among the surgical possibilities are:
- Core Decompression: To increase blood supply to the damaged bone, the surgeon will drill tiny holes, or cores, into your afflicted bone. To help with recovery, this technique may be coupled with injections or bone transplants.
- Bone Grafting: In advanced cases, bone grafts may be used to help repair or strengthen the affected bone. This involves transplanting healthy bone tissue to the damaged area.
- Joint Replacement: For severe cases where the joint is significantly damaged, joint replacement surgery may be necessary to relieve pain and restore function. In this procedure, a prosthetic joint is installed in place of your injured one. In patients with avascular necrosis, hip and knee replacements are 95% successful in reducing pain and increasing mobility.
How is Avascular Necrosis Diagnosed?
Diagnosing avascular necrosis (AVN) involves a combination of medical history review, physical examination, and imaging tests to assess the affected joint and confirm the presence of bone tissue damage. The diagnostic process typically includes:
Medical History and Physical Examination: The doctor will inquire about symptoms, medical history, medications, and any past injuries or treatments. A doctor or nurse will examine your joints during a physical examination to check for any soreness. In order to determine if the range of motion is reduced, they may also rotate the joints through various positions.
Imaging Tests: Various imaging techniques are employed to examine the affected bone and assess its condition:
- X-rays: These can reveal changes in bone structure, such as bone damage or joint collapse.
- MRI (Magnetic Resonance Imaging): Provides detailed images of soft tissues and can detect early signs of AVN, including bone changes and damage to surrounding structures.
- CT (Computed Tomography) Scan: Offers detailed cross-sectional images of bones, helping to identify bone deterioration.
- Bone Scans: A nuclear medicine technique where a small amount of radioactive material is injected into the bloodstream. This material collects in areas of high bone turnover, showing areas where blood supply to bones is disrupted.
Biopsy: In rare cases, a sample of bone tissue may be extracted and examined under a microscope to confirm AVN diagnosis, although this is less commonly performed due to the accuracy of imaging tests.
What are the Risk Factors for Osteonecrosis?
Several factors increase the risk of developing osteonecrosis. Understanding these risk factors is crucial in identifying individuals who might be more susceptible:
- Injury
- Steroid use
- Alcohol use
- Blood disorders, such as sickle cell anaemia
- Gaucher disease
- Caisson disease
- HIV
- Chemotherapy
- Pancreatitis
- Decompression disease
- Hypercoagulable state
- Hyperlipidemia
- Autoimmune disease
- Radiation treatments
How to Prevent Avascular Necrosis?
Preventing avascular necrosis (AVN) involves addressing underlying risk factors and adopting proactive measures to safeguard bone health and circulation. Consider these strategies to help reduce the risk:
- If possible, avoid prolonged or high-dose steroid medications. Discuss alternative treatment options or dosage adjustments with a doctor.
- Limit excessive alcohol intake, as heavy and prolonged use can weaken bones and impair blood circulation, particularly in the hip joint.
- Regular exercise, a balanced diet rich in calcium and vitamin D, and avoiding smoking can promote overall bone health and circulation.
- Take precautions to avoid joint injuries or trauma. Protective gear during high-risk activities or sports can help reduce the likelihood of joint damage.
- If there’s a family history or increased risk due to certain treatments, consult healthcare professionals for guidance and regular monitoring to detect any early signs of AVN.
Understanding AVN Stages
AVN progresses through stages that indicate the severity of the condition. Early detection and intervention are crucial for successful treatment. Here are the stages of AVN:
1. Initial Stage: In this stage, the blood supply to the femoral head is compromised, leading to cellular damage. At this point, the bone structure remains intact, and symptoms might not be noticeable. However, early diagnosis through imaging (X-rays, MRI) can identify subtle changes, enabling timely intervention.
2. Necrosis Stage: Blood flow continues to be restricted, causing the bone tissue to die (necrosis). Patients may start experiencing pain and discomfort during this stage, particularly with weight-bearing activities. Conservative treatments, such as medication, rest, and limited weight-bearing, might be recommended.
3. Crescent Stage: The dead bone weakens and might collapse, leading to a crescent-shaped fracture. Pain and limited range of motion become more pronounced. Surgical interventions, such as core decompression, may be considered at this point to alleviate symptoms and prevent further damage.
4. Flattening Stage: The femoral head loses its shape and flattens due to the ongoing collapse. Joint function significantly deteriorates, leading to more intense pain and reduced mobility. Joint-replacement surgery may be advised to restore function and relieve pain.
5. Advanced Stage: The final stage involves extensive damage to the femoral head, causing severe pain, disability, and joint dysfunction. Total hip replacement surgery becomes a more likely option to restore mobility and quality of life.
Seeking Timely Treatment in India
In India, timely treatment of AVN is of paramount importance, considering the prevalence of conditions that may contribute to AVN, such as trauma, corticosteroid use, alcoholism, and certain medical conditions. If you experience persistent hip pain, limited range of motion, or discomfort during movement, it’s crucial to consult a qualified orthopedic specialist.
Prompt diagnosis through medical imaging and comprehensive evaluation can determine the stage of AVN and guide appropriate treatment. Depending on the stage, treatment options may include medication, lifestyle modifications, physical therapy, core decompression, joint-preserving surgeries, or hip replacement.
Direct Anterior Approach: Revolutionizing Total Hip Replacement
When AVN progresses to the point where joint-preserving treatments are no longer effective, hip replacement surgery becomes a viable option. In recent years, the Direct Anterior Approach (DAA) to hip replacement has gained prominence as a superior surgical alternative in India.
Advantages of DAA Over Conventional Approaches
1. Minimal Muscle Disruption: DAA allows surgeons to access the hip joint without detaching major muscles. This results in less tissue damage reduced post-operative pain, and faster recovery.
2. Preservation of Tissues: DAA enables the preservation of key structures, reducing the risk of complications and enhancing the overall stability of the new hip joint.
3. Accelerated Recovery: Patients undergoing DAA often experience a quicker return to daily activities and improved functional outcomes, making it an excellent choice for those seeking early rehabilitation and mobility.
Conclusion
AVN of the femoral head is a progressive condition that demands timely attention to prevent irreversible joint damage. For those in India, seeking treatment from experienced orthopedic specialists is vital to diagnose and manage the condition effectively. The Direct Anterior Approach to hip replacement stands as an advanced surgical option, offering improved outcomes and faster recovery for patients dealing with advanced stages of AVN. Remember, informed decision-making and proactive healthcare measures are key to maintaining hip health and ensuring a high quality of the life.
FAQs on Avascular Necrosis
Q. Can AVN heal without surgery?
In some cases, especially in its early stages, avascular necrosis (AVN) can potentially heal without surgery, if detected early. Non-surgical treatments like medication, physical therapy, and lifestyle modifications may help manage symptoms and promote healing by improving blood flow and reducing stress on the affected bone. However, advanced stages or severe cases may often require surgical intervention to prevent further damage and restore joint function.