World Food Day: 16 October, 2024
The World Food Day is celebrated on October 16 every year to emphasise the importance of food security worldwide. This day has been chosen to raise awareness about global food and hunger issues. World Food Day was established by the Food and Agriculture Organisation (FAO) of the United Nations (UN) in 1979. This day is celebrated in 150 countries and in 50 languages, making it one of the most significant international events on the UN calendar. World Food Day, also known as International Food Day, provides an opportunity to advocate for food production, procurement, and protection while combating food wastage on a global scale. History of World Food Day The Food and Agriculture Organisation was founded in 1945, and in honour of its establishment, the United Nations designated October 16 as International Food Day or World Food Day during the 20th General Conference in November 1979. Today, governments and organisations worldwide celebrate World Food Day to raise awareness about the critical importance of food security. World Food Day Theme 2024 Since its establishment, the FAO has emphasised the importance of agriculture and food security. Water is an essential element of life; without water, life wouldn’t exist. To emphasise the importance of water in everyday life, the World Food Day theme for 2024 is “Water is Food, Water is Life – Leave No One Behind.” Groundwater reserves and freshwater availability are decreasing day by day. The theme of World Food Day reinforces the importance of reducing water wastage and reusing water, as it is the main source of food and life on Earth. Significance of World Food Day 2024 The Food and Agriculture Organization launched World Food Day as part of its mission to end hunger and advance sustainable agriculture. Raising awareness – World Food Day is an opportunity to raise awareness about food-related concerns. Hunger, food waste, and the need for ecologically sound agriculture are among the primary issues raised on this day. Promoting change – The day provides governments, groups, and individuals with a chance to promote measures aimed at reducing hunger and enhancing food security. Highlighting accomplishments – World Food Day offers a chance to acknowledge and celebrate the strides made in overcoming agriculture and food security challenges. World Food Day in India World Food Day is celebrated with zeal and passion in India. This day is particularly important due to the nation’s agricultural history and the significance of food in Indian culture. On this day, several public and private organisations run awareness campaigns and educational initiatives. Numerous colleges, institutions, and community organisations hold food donation drives to help those in need. Conferences and seminars are held to discuss food security, sustainable agriculture, and cutting-edge agricultural practices. Empowering Food Security Farmers are encouraged to engage in non-crop agriculture to protect themselves from a loss of revenue. Minimising food waste and losses helps keep the supply stable even when overall output is down. Early warning systems, sensors, and drones are technological instruments that should be deployed because they can assist governments and farmers in making better decisions. Distress can be reduced through improved insurance policies for livestock and crops, as well as providing quick relief following natural disasters. Encouraging the development of salt, flood, and drought-resistant seed varieties, as well as native hardy types like coarse cereals, is essential. On World Food Day, we should promote crop diversification by moving beyond the current monoculture practice towards a more varied agricultural approach. Wockhardt Hospitals is dedicated to promoting health and well-being not only within the walls of our healthcare facilities but also in the communities we serve. As a healthcare institution, we understand the vital connection between food, nutrition, and health. On World Food Day, let’s reiterate our commitment to a world where everyone has access to better, more plentiful food. Together, we can nourish our planet and secure a brighter future for generations to come.
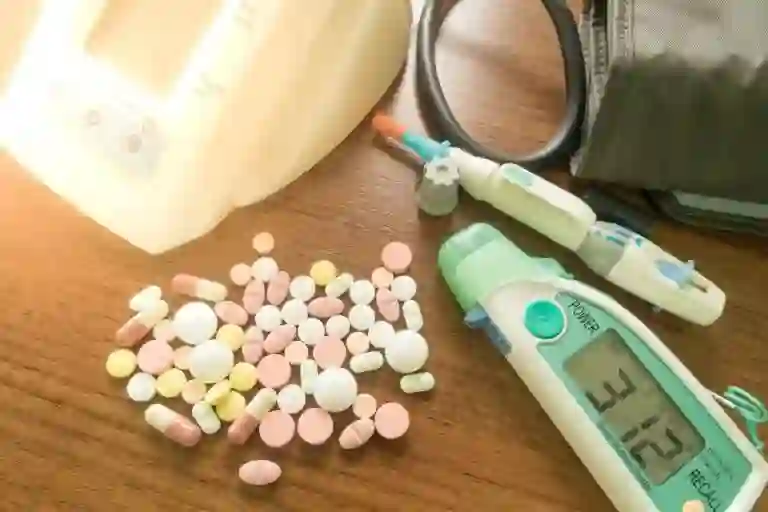
Diabetes Insipidus: Symptoms, Diagnosis & Treatment
Diabetes Insipidus, also known as Diabetic Insipidus, is a rare, serious medical condition and requires comprehensive medical treatment. In Diabetes Insipidus, the body produces excessive amounts of urine and cannot properly store water. It is why the patients consume excessive amounts of water due to persistent thirst caused by lack of water in the body. Diabetes Insipidus is primarily caused by an imbalance in the production of a hormone known as Antidiuretic Hormone (ADH). This imbalance occurs when either the body doesn’t produce enough ADH or the kidneys do not utilize ADH effectively. It can be long-term or short-term, mild or severe, depending on the underlying cause. It is to be noted that although the terms “Diabetes Insipidus” and “Diabetes Mellitus” may sound similar, they are not related. Diabetes Mellitus is a medical condition that is characterized by elevated blood glucose levels. It is a relatively common condition and is often referred to as simply diabetes. Types of Diabetes Insipidus Central Diabetes Insipidus Central Diabetes Insipidus can be a hereditary condition or the result of damage to the hypothalamus, pituitary, or Hypothalamic-Pituitary-Adrenal (HPA) gland. A surgical procedure, tumor, head injury, or other medical condition can lead to such a condition. The damage to the hormone production, storage, and release of the hormone ADH has a direct impact on the condition. Additionally, the condition may be caused by an autoimmune response causing your immune system to attack the cells that produce ADH. Nephrogenic Diabetes Insipidus This disorder is caused by an underlying kidney disorder that impedes the proper functioning of ADH. Kidney disorders can be hereditary, the result of a chronic kidney disorder, or the result of the administration of antiviral drugs. Gestational Diabetes Insipidus It is a rare condition that is only present in pregnant women. It is caused by an enzyme produced by the placenta that destroys ADH in pregnant women. Primary Polydipsia Dipsogenic Diabetes Insipidus is another name for Primary Polydipsia, which is characterized by persistent thirst and excessive fluid consumption. It can be attributed to damage to the hypothalamic system responsible for regulating thirst. Additionally, this condition has been associated with mental health issues, including Schizophrenia. How is Diabetes Insipidus diagnosed? For Diabetes Insipidus diagnosis, our world-class physicians at Wockhardt Hospitals may perform a variety of medical tests. Additionally, they may determine the type of diabetes and the underlying cause of the condition. Diabetes Insipidus diagnosis can be done by taking certain tests, such as: What is Diabetes Insipidus Treatment? In Diabetes Insipidus disease, there is no effective treatment for the condition. However, there is a dedicated treatment available that can reduce the symptoms of the condition, such as thirst, reduced urine output, and dehydration. Diabetes Insipidus can be treated in various ways depending on the severity of the condition. If the condition is mild, the individual may only require additional water intake to prevent dehydration. Diabetes Insipidus treatment varies depending on the type of diabetes a person has. Central Diabetes Insipidus – If the underlying cause of Central Diabetes Insipidus is a malfunctioning pituitary or hypothalamic gland, such as a malignant tumor, it is typically treated at first. However, when additional treatment is necessary, a hormone, desmopressin or DDAVP (Nocdurna), is produced to replace the missing ADH and to reduce the amount of urine produced by the body. DDAVP is available in the form of a pill, a nasal spray, and a shot. Nephrogenic Diabetic Insipidus – The treatment of this condition can be more complex and challenging. If the condition is due to a medicine, discontinuation of the medication may be beneficial. Replacing the medications may also reduce the symptoms. The healthcare provider may suggest the patient consume a diet with a low salt content in order to reduce the amount of urine produced by the kidneys. Treatment with Microzide (Hydrochlorothiazide) may be beneficial in alleviating the symptoms. Hydrochlorothiazide, a diuretic, causes the body to produce more urine; however, it can reduce urine output in some individuals suffering from Nephrogenic Diabetic Insipidus. Gestational Diabetes Insipidus – Desmopressin is a hormone produced by the human body that is used as a treatment for Gestational Diabetes Insipidus. Most of the time, Gestational Diabetes Insipidus disappears after the birth of the baby, but it can return if the mom becomes pregnant again. Primary Polydipsia – There is no treatment for this type of diabetic insufficiency. The only thing one can do is reduce their fluid intake. If diabetes insufficiency is linked to a mental health condition, treatment may reduce symptoms. Lifestyle Modifications for Individuals with Diabetes Insipidus In order to effectively manage and treat Diabetes Insipidus disease, lifestyle changes can be beneficial. One of the most important steps is to prevent dehydration. This can be achieved by taking water with one’s daily routine. The physician will advise on the amount of fluid to be consumed each day. Additionally, regular physical activity, a nutritious diet, quality sleep, and abstaining from smoking can all contribute to overall health. The doctor may also suggest a specific diet that is low in sodium and protein. Diabetes Insipidus can last a lifetime; however, an individual will be able to control their symptoms through regular monitoring and regular fluid intake. By adhering to the guidelines of their health care provider and managing their symptoms, the majority of individuals diagnosed with Diabetes Insipidus are able to avoid severe complications and lead a normal life. Diabetes Insipidus patients should seek immediate medical attention if they experience sudden dizziness or disorientation. Wockhardt Hospital’s Diabetes & Endocrinology Department is one of India’s leading hormonal health practices. We provide comprehensive end-to-end treatment and diagnostics for all hormonal disorders. Schedule an appointment with us to manage your condition effectively.
Discovering the Health Benefits and Delicious Recipes of Watermelon

Remember those summer holidays when you would come home to freshly served slices of cool and sweet watermelon after a game of hide and seek with your friends? Watermelons are not just good for replenishing fluids; they have several health benefits and provide great nutritional value to prevent various health problems. It can even help manage diabetes and help in your weight loss journey while preventing the risk of developing heart disease and asthma. Did you know that watermelon contains a whopping 92% water content with each bite you take? Not only does it give you a boost of freshness and hydration, but it also helps avoid overeating by giving you a feeling of fullness. Containing less than 45 calories, it is a super healthy fruit that everyone can enjoy. Nutritional Benefits of Watermelon for Your Health Watermelon is a hydrating, micronutrient-rich fruit containing a host of nutrients that do good to your health. Apart from being an excellent hydrating agent, it imparts numerous health benefits while supporting weight loss. Watermelon is mostly water and due to its property of giving you a feeling of fullness, it helps to avoid unhealthy snacking while still providing the essential nutrients and just enough calories. Watermelons are also helpful in fighting inflammation, thereby preventing many serious diseases. Not just that, you can say bye to your gum problems if you just add some watermelon to your diet! Delicious and Healthy Watermelon Recipes to Try Today Consuming watermelon every day may not be exactly a party situation for your taste buds, but incorporating this nutrient-dense fruit in various delicious recipes can surely leave your taste buds craving for more! Before we move on, did you know that watermelon is a cent percent edible? Sounds pretty interesting, right? The tough rind contains low levels of calories, but high concentrations of Vitamin C, Vitamin A, and Potassium attributing to improving heart and skin health and enhanced immune function. It’s also nutrient-dense, containing high amounts of citrulline, lycopene, amino acids, flavonoids, and phenolic compounds that reduce oxidation and inflammation. Watermelon seeds — dried or raw — are rich in magnesium and folate. Seeds also have the types of fatty acids that lower bad cholesterol in the blood and help avoid heart attack and stroke. Now that you know, save those pulps, rinds, and seeds for a perfectly healthy recipe. Oh, you’re here for one? Let’s get cooking, then! What comes to mind when you hear about healthy food? Salad, leafy greens, perhaps some fruits (watermelon, anyone?) But how do you make salad appetizing? Well, of course, cheese makes everything better! The best kind of cheese that goes with salad is feta cheese. Here’s how to make a delicious feta salad with watermelon. Ingredients: How to Make Water Melon Feta Salad Step 1: Whisk the vinegar, oil, and salt together in a bowl. Step 2: Add the watermelon and cucumber slices, and mix them with mint, onions, and feta cheese. Step 3: Garnish with more mint and salt, and enjoy! Make your childhood favorite homemade watermelon popsicles now and relive your days of childhood! Ingredients: Steps to Make Step 1: Blend the strawberries and watermelon slices in a blender by adding lime juice, sugar, and salt it. Step 2: After blending it nicely, take out the mixture put it in a freezer mold, and put it in the deep freezer for 6 hours. Step 3: Take out the mold, thaw a little, and your watermelon popsicle is ready! To step up your foodie A-game with watermelons, add a little Mexican twist and make a healthy salsa with watermelon to devour those crispy chips. Ingredients Making salsa is pretty easy. Simply take all the ingredients and mix them in a bowl, and it’s ready to serve! You can also keep it refrigerated for up to 2 days by covering the bowl with a wrap. Watermelon rind can be used in numerous ways and adjusted to make your favorite South Indian food. Watermelon rind is easy to grind and easy to store. So you can have it ready to mix and whip up a curry or dosa/idli/rice in just a few minutes! How to make watermelon rind: After using the watermelon, scrap the fruit part completely, and then cut it into small wedges. Put all the slices in a blender or keep them refrigerated as it is for future use. Ingredients How to Make Watermelon Rind Curry/ Stir fry/ Dosa Step 1: Wash and soak the rice for 3 hours. Grind it in ice water until smooth. Step 2: Blend the watermelon rind without water. Step 3: Transfer the blended rind and rice and set aside for fermentation for 8 hours. If you want to make curry, keep some watermelon rind aside. Step 4: Use the batter for making dosa or idli. Add the remaining watermelon rind to any curry you wish to make. Watermelon seeds are an excellent source of essential nutrients that can be directly consumed or mixed in smoothies and breakfast cereals. Roasted watermelon seeds taste like caramel and add a salty crunch to your food. Now that you know how to use watermelon with zero waste, use the MVP of summer fruit to add a twist to your diet and pair perfectly with basically every summer meal!
Are you feeling dizzy?
It is very common to encounter patients presenting with dizziness or ‘chakkar’ in Neurology OPD but what patients perceive or mean by dizziness varies from patient to patient. It can be a manifestation of innocuous condition such as transient low sugars or may signal something as sinister as a brain stroke or a cardiac problem. Common underlying conditions that can result in dizziness: Considering the varied perceptions of dizziness in different patients and the underlying causes varying from relatively benign to grave, it is important that patients having the above symptoms should seek consultation from Neurologist at the earliest. Timely evaluation and treatment can not only relieve the patient of disabling symptoms but can also result in improved prognosis in patients with severe underlying causes. Dr. Prashant MakhijaMBBS, MD (Medicine)DM (Neurology), PDF Epilepsy & Sleep MedicineConsultant Neurologist, Wockhardt Hospitals, Mumbai Central
Innovative Hip Replacement Surgery Using Direct Anterior Approach (DAA)

In the world of orthopedic surgery, each case presents its unique challenges and opportunities for innovation. One such case that remains etched in my memory is that of a young patient named Minesh, who had Down Syndrome and was suffering from Avascular Necrosis (AVN) of the hip. Minesh’s journey began with a diagnosis that no one wants to hear—AVN of the hip. This condition, characterized by the loss of blood supply to the hip joint, can be excruciatingly painful and debilitating. What made Minesh’s situation even more complex was his diagnosis of Down Syndrome, a genetic disorder that posed its own set of challenges. Typically, patients undergoing Total Hip Replacement (THR) surgery must follow strict post-operative precautions to prevent dislocation of the new hip joint. However, patients with Down Syndrome often face cognitive and physical limitations that make adhering to these precautions extremely challenging. As an orthopedic surgeon of Minesh, I faced the task of not only addressing his AVN but also finding a solution that would accommodate his unique needs. After a thorough evaluation and discussions with his family, I decided to take an innovative approach—the Direct Anterior Approach (DAA). The Direct Anterior Approach (DAA) is a minimally invasive surgical technique that provides access to the hip joint without detaching muscles or tendons. This approach significantly reduces the risk of post-operative hip dislocation and eliminates the need for strict hip precautions. For Minesh, it offered the potential for a smoother recovery and improved post-operative experience. The day of the surgery arrived, and our team at Wockhardt Hospitals was ready. With precision and care, we performed the THR using the Direct Anterior Approach (DAA). The procedure went smoothly, and Minesh was on his way to recovery. What followed was nothing short of remarkable. Minesh’s rehabilitation process was more manageable than we had anticipated. He faced fewer post-operative challenges, and his journey toward regaining mobility and independence started sooner than expected. Minesh’s case highlighted the importance of tailoring medical care to individual patient needs, especially in cases where traditional approaches may not be suitable. It also emphasized the power of innovation in the field of orthopedics, enabling us to provide the best possible care for patients like Minesh. As an orthopedic surgeon, it’s moments like these that remind me why I chose this profession. Witnessing the positive impact of our decisions on a patient’s life is truly rewarding. Minesh’s story serves as a testament to the resilience of the human spirit and the possibilities that emerge when we combine medical expertise with innovative solutions. At Wockhardt Hospitals, we remain committed to providing patient-centered care and embracing advancements in the field to ensure that every patient’s journey to recovery is as smooth and successful as possible. Dr. Supreet BajwaOrthopedic & Joint Replacement SurgeonWockhardt Hospitals, Mumbai Central
Heart Valve Surgery: Repair & Replacement
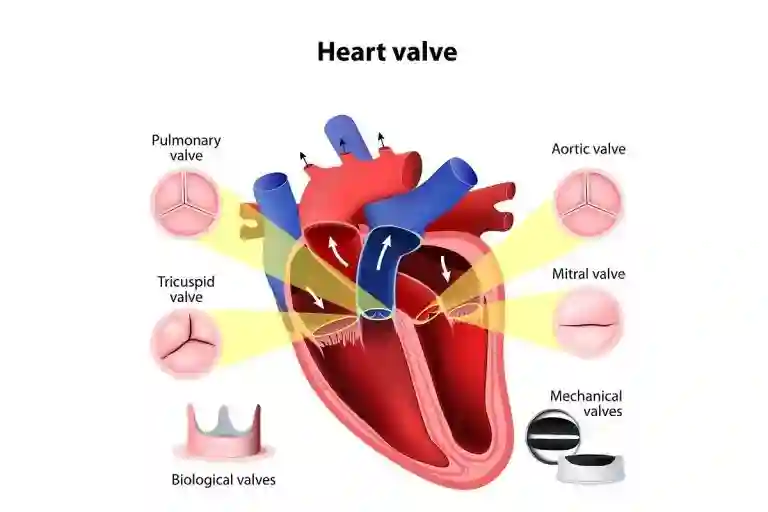
Heart valve surgery and procedures are performed to repair or replace a valve in the heart that is not working properly because of valvular heart disease (also called heart valve disease). Heart valve replacement surgery is open-heart surgery through the breastbone, into the chest. It is a major operation that can last two hours or longer and recovery often takes several weeks. There are newer, less invasive procedures suitable for some types of valvular heart diseases. Why is it Done? In a healthy heart, valves control the flow of blood by making it move in one direction through the heart and the body. The valve can either become stenotic, which means it is narrowed and thus does not allow the blood to flow smoothly from one chamber to another or it starts leaking which hampers the forward flow of blood. If your valve problem is minor, your doctor may monitor your symptoms or treat you with medication. If your condition is more serious, surgery is usually required to repair or replace the valve to prevent any lasting damage to your heart valve and your heart. What is Done? Depending on the problem, there are several different procedures for repairing or replacing valves. 1. Surgical Valve Repair Surgical procedures are generally used for problems with the mitral or tricuspid valves. 2. Commissurotomy It is a treatment for a tight valve. The valve flaps (leaflets) are cut to loosen the valve slightly, allowing blood to pass easily. 3. Annuloplasty It is done for a leaky valve. There is a ring of fibrous tissue at the base of the heart valve called the annulus. To repair an enlarged annulus, sutures are sewn around the ring to make the opening smaller. Or, a ring-like device is attached around the outside of the valve opening to support the valve so it can close more tightly. 4. Valvulotomy It is a procedure to enlarge narrowed heart valves. It can also be done with the help of a balloon. 5. Non-Surgical Valve Repair Percutaneous or catheter-based procedures are done without any incisions in the chest or stopping the heart. Instead, a thin flexible tube called a catheter is inserted into a blood vessel in your groin or arm and then threaded through the blood vessels into your heart. Percutaneous or balloon valvuloplasty/valvotomy is used for stiffened or narrowed (stenosed) pulmonary, mitral, or aortic valves. A balloon tip on the end of the catheter is positioned in the narrowed valve and inflated to enlarge the opening. Percutaneous mitral valve repair methods – such as edge-to-edge repair – can fix a leaky mitral valve in a patient who is considered at high risk for surgery. A catheter holding a clip is inserted into the groin and up into the left side of the heart. The open clip is positioned beyond the leaky valve and then pulled back so it catches the flaps (leaflets) of the mitral valve. Once closed, the clip holds the leaflets together and stops the valve from leaking
Difference Between Acute and Chronic Kidney Failure
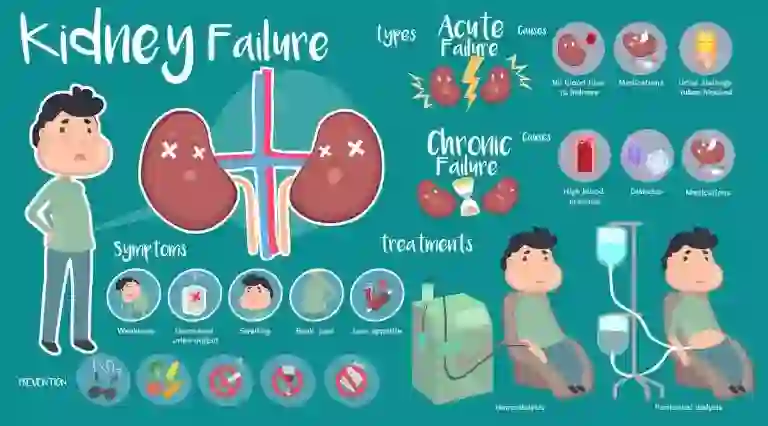
Currently, there is a growing awareness surrounding kidney health. If the kidneys fail to filter the waste effectively, a situation known as kidney failure arises. When the kidneys cannot properly filter the blood, wastes accumulate in them, which upsets the balance of the chemical constituents. Kidney failure, whether acute or chronic, varies in length, onset, and reversibility. Kidney function rapidly declines as a result of acute renal failure, which happens unexpectedly and is frequently caused by an injury or infection. Usually, it can be reversed with quick medical attention. On the other hand, chronic kidney failure occurs gradually over months or years and is frequently brought on by diseases like diabetes or high blood pressure. As irreversible damage builds up, renal function eventually declines permanently. What is the Difference Between Acute and Chronic Kidney Failure? Chronic kidney disease (CKD) and acute kidney injury (AKI) vary in several important ways: Acute Kidney Failure Chronic Kidney Failure Usually brought on by a medication, disease, or trauma Usually brought on by a long-term sickness Kidney function declines rapidly. Kidney function declines gradually The symptoms appear suddenly and may be quite serious. Until the damage is severe, symptoms might not show up. The goal of the treatment is to address the underlying reason. The goal of the treatment is to manage the underlying problem. Often reversible with prompt treatment. Irreversible, focuses on slowing further deterioration. Symptoms and Causes of Acute Kidney Failure Acute kidney failure signs and indicators might include: A sudden reduction in urine production. Urine may seem darker than usual or frothy or foamy due to excess of protein in the urine. Decreased kidney function results in the body accumulating fluid, which is seen as swelling. The retention of fluids is the reason for the abrupt weight increase. Breathing problems may arise from an accumulation of fluid in the lungs. Fatigue and lethargic mood. Feelings of helplessness and trouble concentrating. Vomiting and nausea. Abnormal heart rhythm or palpitations. Twitches and spasms of muscles. Abdominal pain or discomfort. Skin itching. In extreme circumstances, seizures or coma. Causes of Acute Kidney Failure Include: Insufficient fluid intake that leads to dehydration. Excessive loss of fluids due to vomiting, diarrhea, or sweating. The kidneys may be affected by an inflammatory response brought on by severe infection. Kidney-damaging urinary tract infections. Prolonged or high-dose NSAID. Medications used in imaging tests, such as dyes, antibiotics, and certain chemotherapeutic medications. Liver dysfunction can impact blood volume and renal blood flow. Blood clot in the kidneys’ blood vessels or Thrombosis can impede blood supply to the kidneys. Direct injury to the tissues of the kidneys might result from physical trauma. Kidney injury could arise from stones obstructing the urine system. Blood flow to the kidneys may be compromised by decreased cardiac output. Symptoms and Causes of Chronic Kidney Failure In cases where kidney damage advances slowly, signs and symptoms of chronic kidney failure gradually appear. An accumulation of fluid, bodily waste, or electrolyte imbalances can result from renal failure. Depending on the extent, kidney function loss might result in: Nausea Weakness and exhaustion Vomiting Decreased appetite Unintentional weight loss Sleep issues Elevated or lowered urine production Impaired cognitive function Continuous itching Parched and discolored skin Uncontrollably high blood pressure, or hypertension Breathing difficulties if a buildup of fluid occurs in the lungs Chest discomfort in the event that fluid accumulates around the heart’s lining When a sickness or disease affects kidney function, kidney damage worsens over a period of months or years, leading to chronic kidney disease. The following diseases and conditions can result in chronic kidney disease: Unregulated blood sugar levels. Persistently high blood pressure. An inflammation of the kidney’s filtration units, or glomeruli, is known as glomerulonephritis. Kidney tubule and surrounding structural inflammation, known as interstitial nephritis. Kidney diseases that are hereditary, such as polycystic kidney disease. Inflammation of the kidney’s tubules and surrounding structures. Extended use of nephrotoxic medications, such as NSAIDs. History of kidney disease in the family. Pyelonephritis, or recurrent kidney infection. Prolonged blockage of the urinary tract caused by diseases such kidney stones, enlarged prostates, and some malignancies. Treatment of Acute Kidney Failure Acute kidney failure usually requires hospitalization for treatment. The duration of your hospital stay depends on the cause of your acute kidney damage and the speed at which your kidneys heal. In certain situations, you may be able to recuperate at home. The treatment of acute kidney failure focuses on addressing the underlying cause, supporting kidney function, and preventing complications. The main aspects of treatment include: Fluid Replacement: This involves treatments aimed at achieving a balanced blood fluid level. If dehydration is the primary cause of your acute kidney damage, your doctor may recommend intravenous (IV) fluids. Medications to Control Blood Potassium: Your doctor may suggest calcium, glucose, or sodium polystyrene sulfonate (Kionex) if your kidneys are not effectively filtering potassium from your blood, preventing excessive potassium levels from accumulating. Blood Calcium Levels: If your blood calcium levels become too low, your doctor may recommend a calcium infusion. Dialysis: Temporary hemodialysis, also known as dialysis, may be necessary to flush out toxins and extra fluid from your body while your kidneys heal. You might not need to follow a particular diet once your kidneys heal, but eating healthily is still crucial. Treatment of Chronic Kidney Failure While there is no cure for chronic kidney disease (CKD), you can live a much longer life with healthy, working Kidneys. Medication Management: You may be prescribed one or more medications to control underlying conditions causing kidney failure, such as hypertension or diabetes. A doctor may recommend medication to reduce blood pressure since kidney failure and high blood pressure are connected. It’s possible that you’ll also require statins to reduce your cholesterol. Fluid Control: If you are experiencing fluid retention due to a renal disease, diuretics can help reduce swelling. Strict control of fluid intake to prevent fluid overload and maintain a balance. Dialysis: When your kidneys will no longer be able to eliminate
What is a Coronary Artery Bypass Graft?
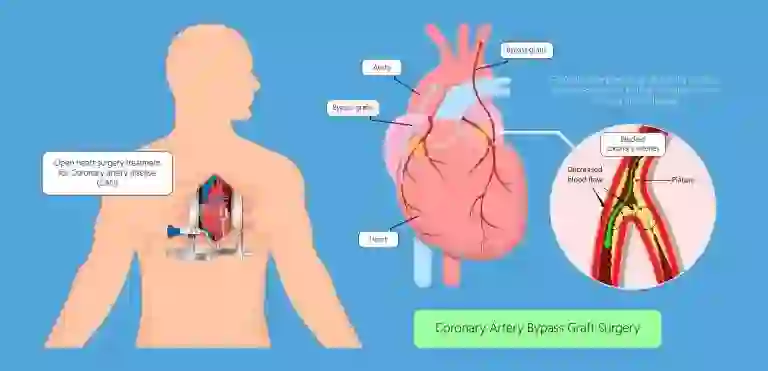
A coronary artery bypass graft (CABG) is a surgical procedure used to treat coronary heart disease. It diverts blood around narrowed or clogged parts of the major arteries to improve blood flow and oxygen supply to the heart. Why is it Carried Out? Like all organs in the body, the heart needs a constant supply of blood. This is supplied by 2 large blood vessels called the left and right coronary arteries Over time, these arteries can become narrowed and hardened by the build-up of fatty deposits called plaques. Your chances of developing coronary heart disease increase with age, you are also much more likely to be affected if: Coronary heart disease can cause angina, which is chest pain that happens when the supply of oxygen-rich blood to the heart becomes restricted. Another risk associated with coronary heart disease is the possibility of one of the plaques in the coronary artery rupturing (splitting), creating a blood clot. If the blood clot blocks the blood supply to the heart, it can trigger a heart attack. A coronary artery bypass graft may be recommended to reduce your chances of having a heart attack. Procedure for Coronary Artery Bypass Graft A coronary artery bypass graft involves taking a blood vessel from another part of the body (usually the chest, leg, or arm) and attaching it to the coronary artery above and below the narrowed area or blockage. This new blood vessel is known as a graft. The number of grafts needed will depend on how severe your coronary heart disease is and how many of the coronary blood vessels are narrowed. A coronary artery bypass graft is carried out under general anesthetic, which means you’ll be unconscious during the operation. It usually takes between 3 and 6 hours. Recovery After Surgery Most people will need to stay in the hospital for about 6 to 8 days after having a coronary artery bypass graft. Recovery takes time and everyone recovers at slightly different speeds. Generally, you should be able to sit in a chair after 1 day, walk after 3 days, and walk up and down stairs after 5 or 6 days. When you go home, you’ll need to take things easy for a few weeks. You should be able to return to most of your normal activities after about 6 weeks. After Treatment How to Take Care of Your Body After having a coronary artery bypass graft, most people will experience a significant improvement in symptoms such as breathlessness and chest pain, and their heart attack risk will be lowered. But a coronary artery bypass graft isn’t a cure for coronary heart disease. If you don’t make lifestyle changes, such as eating a healthy diet and exercising regularly, your grafted arteries will also eventually become hardened and narrowed.
A Challenging Journey of a Postman…Towards Recovery
Prashant Yelawande, a 56-year-old postman employed by the central government, presented with multiple health issues requiring medical intervention. Prashant initially reported severe pain in the lower part of his back, accompanied by difficulty in walking. Dr. Behram Pardiwala examined him and detected tenderness in the lumbosacral spine. Despite an orthopedic surgeon’s opinion that there was no significant issue, Dr. Pardiwala suspected an underlying abnormality. An MRI was performed, revealing the presence of pus in the Psoas region. A general surgeon was consulted to drain the collection. Following the drainage procedure, the patient experienced recurring pain below the left shoulder, which was found to be due to the presence of pus in that area. Dr. Pardiwala suspected an underlying cause for the recurrent infections and ordered further investigation. Comprehensive evaluation revealed that the patient’s tricuspid valve was infected, leading to bacterial endocarditis. The infected tricuspid valve was identified as the source of the recurrent infections and abscesses. Sharing his experience Dr. Behram Pardiwala, Internal Medicine, Wockhardt Hospitals, Mumbai Central mentioned, “Although the surgeon suspected tuberculosis as the possible cause, I insisted on further investigation to determine the source of infection. Upon comprehensive evaluation, it was discovered that the patient’s tricuspid valve was infected. As a result, emboli were being released from the infected valve, leading to the formation of abscesses throughout the body. Once the infected tricuspid valve was identified, it was diagnosed as bacterial endocarditis (Infection of a heart valve).” Antibiotics were initially administered to address the infection in the tricuspid valve. However, despite antibiotic treatment, the infection persisted. Dr. Gulshan Rohra, a cardiac surgeon, was consulted, and it was determined that the patient also had coronary artery disease. Surgical intervention was planned to address both conditions. Surgical procedures performed by Dr. Gulshan Rohra: Dr. Gulshan Rohra, Cardiothoracic Surgeon, Wockhardt Hospitals, Mumbai Central, who operated the patient, said, “Through a comprehensive surgical approach, including removal of the infective mass, tricuspid valve replacement, atrial septal closure, and coronary artery bypass grafting, we were able to successfully address the complex health issues faced by Mr. Prashant Yelawande. The patient’s remarkable recovery and restoration of mobility are a testament to the effectiveness of the surgical interventions. Our collaborative efforts aimed at providing the best possible care and achieving a positive outcome for the patient.” The patient’s surgery and postoperative period were uneventful. He was able to mobilize within the first 48 hours after surgery. Following the completion of the prescribed course of antibiotics, Prashant was discharged from the hospital after a 45-day stay. He made a remarkable recovery, regaining full mobility and being able to walk and engage in regular activities without any limitations. Due to the extensive damage caused by the infection to the heart, it is anticipated that the patient may require a pacemaker in the near future. Further evaluation and planning will be done to address this potential need. Through the collaborative efforts of Dr. Behram Pardiwala and Dr. Gulshan Rohra, Prashant Yelawande’s complex health issues were successfully addressed. The timely diagnosis and appropriate surgical interventions resulted in a positive outcome, allowing the patient to regain his health and normal daily activities. On-going medical care and future considerations will be crucial to ensure his continued well-being. “I faced mountains of challenges, but with unwavering determination and the support of an exceptional medical team of Wockhardt Hospitals, I conquered my complex health issues. My journey has taught me that resilience knows no bounds, and healing is possible against all odds.”
Coping With Diabetes And Hypertension During the Pandemic Era
COVID-19 is a serious public health concern and people with chronic medical issues such as diabetes and hypertension are at a higher risk of getting sick from coronavirus. Here’s how people with diabetes and hypertension should take care of themselves during the pandemic. Follow these guidelines and stay hale and hearty. Coronaviruses (CoV) belong to a large family of viruses that may lead to respiratory illnesses, ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome (MERS-CoV) and Severe Acute Respiratory Syndrome (SARS-CoV). this year, a new strain of coronavirus was discovered, which has not been previously identified in human beings, also known as a novel coronavirus (nCov). COVID-19 causes respiratory disease and in serious cases, it can lead to pneumonia, and hence, the entire country is under lockdown. COVID can affect those with chronic illnesses such as diabetes, high blood pressure, or hypertension as they are in the ‘high-risk’ category. If one gets diabetes, not only his/her blood sugar level gets impacted and the insulin production level also gets compromised. People with high or unmanaged blood sugar levels have less than normal blood flow and their body finds it difficult to harness nutrients and heal. People suffering from diabetes can are prone to develop infections, and may take a longer time to get fit and fine owing to the weakened immune system. Not only this, but uncontrolled blood sugar levels can also invite diabetes-related complications. Similarly, people with hypertension need to be careful. Hypertension can be described as a condition wherein the long-term force of the blood against one’s artery walls is high enough that it may invite major health problems like heart disease and stroke. The risk factors can be attributed to obesity, family history, too much alcohol intake, and smoking. Since people have been advised to stay at home their blood sugar levels and hypertension may go out of control. Hence, they should take charge of their health and stay healthy. Tips for People with Diabetes and High Blood Pressure · Hydrate yourself by drinking enough water, and eat fresh fruits and vegetables to improve your immunity. Dietary Approaches to Stop Hypertension (DASH) diet can also be helpful for people who have hypertension. It also involves whole grains, fresh fruits, vegetables, and low-fat dairy foods. · Monitor your blood sugar levels and temperature from time to time. · Stay in contact with your doctor, and see to it that you have an adequate stock of medication and other supplies for monitoring your blood sugar level at home. If you notice fluctuations then immediately consult the doctor. Do not forget to stock up your insulin if you are advised to take it. · Pay close attention to the changes occurring in the body as that could be a sign of infection. · Try to exercise at home. You can walk, do yoga, or aerobics. Maintain optimum weight. Meditate every day when you feel anxious or tend to panic. · Say NO to high-calorie foods, carbohydrates, too much salt, junk, oily, spicy, and processed foods. · Drinking alcohol on a regular basis can be harmful to your health. It can put you at risk of hypertension. So, limit your alcohol consumption and quit smoking too.