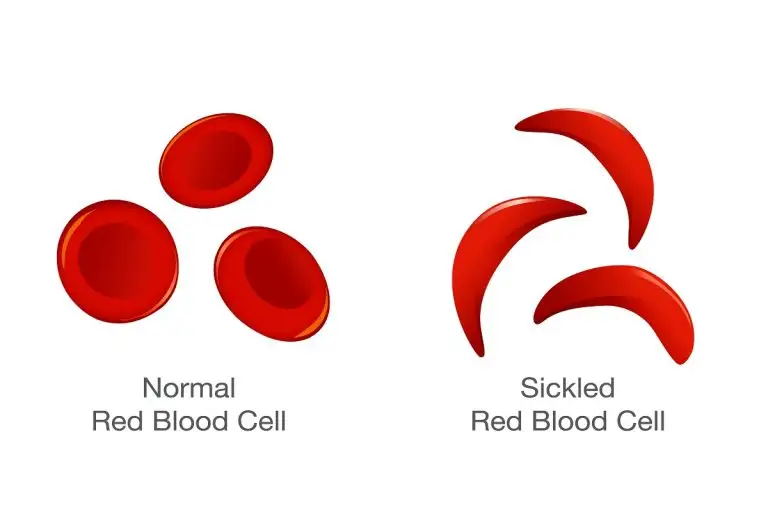
Sickle cell disease is one of the most common inherited blood disorders in which red blood cells become sickle-shaped and sticky in response to low oxygen. It is prevalent mainly in tropical countries. The magnitude of this problem is huge and largely unmet by healthcare as the population affected globally lives in areas with limited resources in terms of healthcare, finances, education. The probability of getting sickle cell disease(SS Pattern) or sickle thalassemia(S/beta thal) is 25% when either both parents are sickle cell carriers (AS pattern) or one sickle cell carrier and the other one is a thalassemia carrier. Sickle cell disease can be very debilitating for the patient as sticky blood can stop blood flow to any organ leading to anything from mild joint pains to clots in the brain, heart attack, liver damage, multiple organ failure simultaneously, and even death. One of the major determinants of any disease control is the identification of carriers. In both sickle cell as well as thalassemia; carriers being asymptomatic, come to know about the disease only after their child gets symptoms and is diagnosed with the disease. In developed countries, this problem is tackled partly by universal screening at birth. In resource-poor countries, the goal should be to aggressively educate the masses and to screen the high-risk population for carrier status by hemoglobin electrophoresis and do prenatal testing at 12 weeks of pregnancy if both parents are affected by either sickle cell or thalassemia. These steps are already in place in some high burden states. In the Indian context, Nationwide screening was conducted by MoTA and ICMR (2016-18): They screened 1.13 crore people, in whom 9.49 lakh carriers and 47311 cases with sickle cell disease were identified. Our sickle cell burden in the tribal population alone is estimated to be >1.8 crore carriers and >13 lakh are estimated to be suffering from sickle cell disease. The states with the highest prevalence are Madhya Pradesh, Maharashtra, Tamil Nadu, Andhra Pradesh, Uttar Pradesh, Gujarat, Kerala, Karnataka, Orissa. After identifying, these subsets of patients need comprehensive medical care at centers specially trained to manage sickle-related complications near their homes. At the very least, the patients should have access to NAT-tested blood and extended phenotype testing should be offered at diagnosis, and blood banks should be able to give ABO, Rh, C,c, E,e, and K antigen matched blood to reduce the risks of transfusion-transmitted infections and alloimmunization respectively, which further burdens the healthcare. We also need to fight misinformation in the community for example not all sickle patients require regular blood transfusions, false concerns regarding the safety of hydroxyurea which is a boon to sickle patients and found safe in long term studies done in sickle patients and reassure them that the increase in bilirubin does not always mean jaundice. In this digital era, we should adequately use social media as a tool to spread awareness in local languages, especially in more affected tribal areas. We need to understand this as everyone’s problem, and common people need to step forward to donate blood, help in awareness, as well as volunteer for various projects from government and NGOs. We have to appreciate that millions of people are already working globally to fight this disease of the underprivileged and it’s high time that, more are sensitized to fight this disease successfully.
By- Dr.Vishvdeep Khushoo
Consultant- Haematologist &Haemato-oncologist